While chemotherapy has advanced in personalization, personalized radiation therapy for cancer remains underdeveloped. A new project will use AI, in particular, deep reinforcement learning, to analyze multimodal data, and enhance cancer characterization and treatment to ultimately improve patient outcomes. Using personal health data, genetic information about the tumor, and patient treatment and follow-up data, digital twins will simulate diagnoses and treatment options to help physicians choose the most effective treatments and monitor responses over time.
Tag: patient outcomes

Cedars-Sinai Again Ranked in Top Tier of U.S. Hospitals
Cedars-Sinai has been named to the Honor Roll for the ninth consecutive year in U.S. News & World Report’s “Best Hospitals 2024-25” rankings.
New Research Supports American College of Surgeons’ Quality Verification Program Standards
Implementing a standardized quality verification program in hospitals can significantly enhance surgical care, as demonstrated by a review study published in the Journal of the American College of Surgeons (JACS). This review provides comprehensive evidence on the positive impact of team-based and disease-based clinical programs, compliance with hospital-level regulatory metrics, and their effect on patient outcomes.
MedStar Washington Hospital Center Again Named the Most Socially Responsible Hospital in the District
MedStar Washington Hospital Center is again the most socially responsible hospital in Washington, D.C. and is among the best in the nation, according to the Lown Institute, an independent think tank. It is ranked #1 in D.C., and is one of 154 hospitals to earn Honor Roll status with “A” grades in all top categories: Social Responsibility, Equity, Value, and Outcomes — key performance metrics that contribute to the overall rating.
Data analysis of electronic medical records can predict adverse outcomes and suggest medications
Electronic medical records (EMRs) are digital versions of the paper charts typically found in clinician offices, clinics, and hospitals and are mostly used by healthcare providers for diagnosis and treatment. New research has leveraged EMR data analysis to predict the risk of developing adverse outcomes in the near future based on an individual’s medical history, and also pinpoint which medications may have beneficial effects.
Replacing Registered Nurses in High Stakes Hospital Care is Dangerous to Patients
A new study published in Medical Care today showed that substituting registered nurses (RN) with lower-wage staff (e.g. licensed practical nurses, unlicensed assistive personnel) in hospital care is linked with more deaths, readmissions, longer hospital stays, poorer patient satisfaction, and higher costs of care.
Study Unveils Balance of AI and Preserving Humanity in Health Care
The survey of more than 1,100 nursing professionals and students shows that more than half express reservations toward the integration of artificial intelligence and 38% question its potential benefits for the nursing field. In addition, despite the potential of telehealth services, 74% of nurses have never utilized them, citing doubts about their efficacy in delivering comprehensive patient care. The new report recommends four strategies for health care organizations to empower nurses in adopting AI.

Joint Accreditation Expands Cedars-Sinai’s Interprofessional Continuing Education
The Continuing Medical Education program at Cedars-Sinai has earned Joint Accreditation with Commendation, enhancing continuing education opportunities for healthcare professionals and signifying that Cedars-Sinai upholds the highest standards in providing relevant, effective, practice-based education.
American Joint Replacement Registry Releases 10th Annual Report
The American Joint Replacement Registry (AJRR), the cornerstone of the American Academy of Orthopaedic Surgeons (AAOS) Registry Program, published its 2023 Annual Report on hip and knee arthroplasty procedural trends and patient outcomes today.
Teamwork interventions may have a positive effect on hospital climate for nurses but do not improve patient outcomes
A pragmatic controlled trial found interventions to redesign care for hospitalized medical patients helped to improve the perceived level of teamwork from nurses’ perspectives but did not seem to affect patient outcomes. According to the authors, health care leaders should consider these findings in the context of their improvement priorities before implementing similar interventions. The study is published in Annals of Internal Medicine.
Tri-City to Partner with UC San Diego Health in Delivering World-Class Medical Care
UC San Diego Health has been selected as Tri-City Healthcare District’s future health care partner.
Surgical Scorecards May Cut Cost of Surgical Procedures Without Impacting Outcomes
A tool for evaluating the overall cost of a surgical procedure, called a scorecard, helps reduce costs of surgical procedures between 5% and 20% without adversely affecting clinical outcomes.
SLU Study: Head and Neck Cancer Diagnostic Delays Linked to Antibiotics Despite Clinical Practice Guidelines
Researchers at Saint Louis University School of Medicine say diagnostic delays frequently occur in patients with undiagnosed head and neck cancer (HNC) and are calling for improved dissemination of current clinical practice guidelines in a new paper published Aug. 24 in JAMA Otolaryngology – Head & Neck Surgery.

MedStar Washington Hospital Center Named the Most Socially and Racially Responsible Hospital in the District
MedStar Washington Hospital Center is the most socially responsible hospital in Washington, D.C. and is among the top in the nation, according to the Lown Institute. The 2023-24 Lown Institute Hospitals Index evaluated more than 3,600 hospitals nationwide, and MedStar Washington ranked #1 in D.C. and is among 54 U.S. hospitals to earn Honor Roll status with “A” grades in all top categories: Social Responsibility, Health Equity, Value of Care, and Patient Outcomes. It also named MedStar Washington the most racially inclusive hospital in the District.
Emergency General Surgery Verification Program Verifies First Five Hospitals
Five hospitals are among the first in the nation to be verified under the new American College of Surgeons Emergency General Surgery Verification Program (ACS EGS-VP) launched in September 2022.

VUMC Joins Group to Accelerate Implementation of Research Findings to Improve Patient Outcomes
The Patient-Centered Outcomes Research Institute (PCORI) is naming Vanderbilt University Medical Center (VUMC) to a select group of health systems nationwide brought together to accelerate the implementation of medical research results that will improve patient outcomes.
Patients and Doctors Agree on Treatment Goals Only Half the Time, According to JNCCN Study on People with Neuroendocrine Tumors
New research in JNCCN finds that only 30% of patients with advanced neuroendocrine tumors (NETs) say their top goal for treatment is living longer. Only 51.7% of patients perceived that they had the same treatment goals as their physician.
Cedars-Sinai Ranked #2 Hospital in Nation by U.S. News & World Report
Cedars-Sinai has been named the #2 hospital in the nation and #1 in California in U.S. News & World Report’s “Best Hospitals 2022-23” rankings.

FAU Awarded $1 Million to Help Prevent Injury, Death from Falls in Older Adults
Every second, an older person in the U.S. falls and injures themselves, and every 20 minutes one of them dies from the fall. The Geriatric Emergency Department Fall Injury Prevention Project will investigate several emergency department-based prevention strategies in older patients at high risk for recurrent falls and injury. The tailored multicomponent intervention will identify effective fall prevention strategies that target limited resources to high-risk individuals who come to the emergency department to improve patient outcomes, improve safety, and reduce overall costs of health care.
Pulmonary Fibrosis Foundation Research Explores Quality and Access to Patient Care
The Pulmonary Fibrosis Foundation announced research results from four studies examining access to care and outcomes for patients living with pulmonary fibrosis and interstitial lung disease.
Hear Us Out Campaign Reports Nurses’ COVID-19 Reality
American Association of Critical-Care Nurses launches Hear Us Out, a nationwide effort to report nurses’ reality from the front lines of the COVID-19 pandemic and urge those who have yet to be vaccinated to reconsider
Hospitals with More Inpatient Nurse Practitioners Linked to Better Outcomes, More Satisfied Patients
According to a new study published today in Medical Care, hospitals that employ more inpatient nurse practitioners (NPs) have lower surgical mortality, higher patient satisfaction, and lower costs of care. Nurse practitioners are registered nurses (RNs) with advanced graduate education and expanded legal scope of practice to prescribe treatments including pain medications.
Schizophrenia Study Suggests Advanced Genetic Scorecard Cannot Predict a Patient’s Fate
Researchers at the Icahn School of Medicine at Mount Sinai found that a tool commonly used in research for evaluating a person’s genetic risk for a disease, called a polygenic risk score, was no better at predicting the outcome of a schizophrenia patient’s disease over time than written reports. The results raise important questions about the use of polygenic risk scores in real-world, clinical situations, and also suggest that a doctor’s written report may be an untapped source of predictive information.
Safe Nurse Staffing Standards in Hospitals Saves Lives and Lowers Costs
A new study published in The Lancet Global Health showed that establishing safe nurse staffing standards in hospitals in Chile could save lives, prevent readmissions, shorten hospital stays, and reduce costs.
New AACN CSI Academy Cohort at 10 Hospitals Focuses on Underserved Patient Populations
Thanks to a grant from Edwards Lifesciences Foundation, nurses caring for underserved critically ill cardiac patients at 10 U.S. hospitals will participate in a cardiac-focused cohort of AACN Clinical Scene Investigator (CSI) Academy, a nurse leadership and innovation program from the American Association of Critical-Care Nurses.
EHR Usability Issues Linked to Nurse Burnout and Patient Outcomes
A new study from the University of Pennsylvania School of Nursing’s Center for Health Outcomes and Policy Research (CHOPR) has investigated associations between EHR usability and nurse job outcomes (burnout, job dissatisfaction, and intention to leave) and surgical patient outcomes (inpatient mortality and 30-day readmission).
More Primary Care Physicians Could Mean Gains in Life Expectancy, Fewer Deaths
New study quantifies the effects of increasing the number of primary care physicians in areas with physician shortages
Increasing the number of primary care physicians in such regions could boost population life expectancy
More primary care physicians could mean fewer deaths in these shortage regions
Nurse Work Environment Influences Stroke Outcomes
Stroke remains a leading cause of death worldwide and one of the most common reasons for disability. While a wide variety of factors influence stroke outcomes, data show that avoiding readmissions and long lengths of stay among ischemic stroke patients has benefits for patients and health care systems alike. Although reduced readmission rates among various medical patients have been associated with better nurse work environments, it is unknown how the work environment might influence readmissions and length of stay for ischemic stroke patients.
New Study Helps Forecast Functional Recovery Time and Return to Activities Following Hip Fracture Surgery
For patients undergoing surgery for a hip fracture, there are still unknowns regarding the return to pre-facture level of function, specifically in regard to driving and mobility. However, a new article published in the January issue of the Journal of the American Academy of Orthopaedic Surgeons® (JAAOS®) further quantifies these outcomes. The study authors found that patients can expect to regain full functionality within two to three years after hip fracture surgery. The study also looked at the long-term psychosocial limitations of patients compared to peer groups and concluded that socialization may aid in recovery.
Total Joint Replacement and the Impact on Future Falls in Osteoarthritis Patients
Patients who have had a total joint arthroplasty (TJA) demonstrate excellent long-term outcomes with increased mobility and improved ability to complete their activities of daily living. However, there is still an ongoing debate whether patients who have undergone TJA are at an increased risk of falls and fragility fractures. According to a new research article published in the Journal of the American Academy of Orthopaedic Surgeons®, authors compared the fall rates of nearly 500,000 cases of osteoarthritic patients and found those who underwent TJA experienced a significantly lower number of falls post-op than those who did not have the surgery.
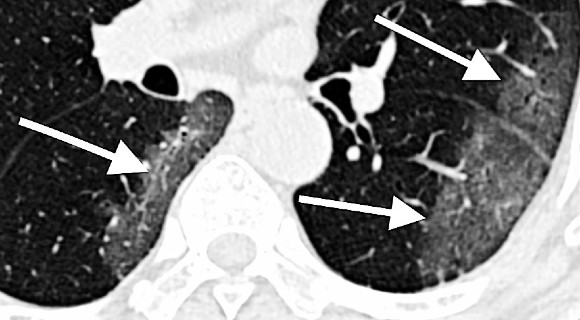
NIH harnesses AI for COVID-19 diagnosis, treatment, and monitoring
NIH has launched an ambitious effort to use artificial intelligence, computation, and medical imaging to enable early disease detection, inform successful treatment strategies, and predict individual disease outcomes of COVID-19.
“Prescribing Art” course teaches med students to recognize bias and better address racial disparities
Can art help doctors better understand their patients and address racial disparities? An innovative collaboration at the University of Alabama at Birmingham uses art to help medical students hone their observational skills, in order to make more accurate diagnoses. “Prescribing Art: How Observation Enhances Medicine” is a partnership between the School of Medicine, the Abroms-Engel Institute for Visual Arts and the Birmingham Civil Rights Institute.
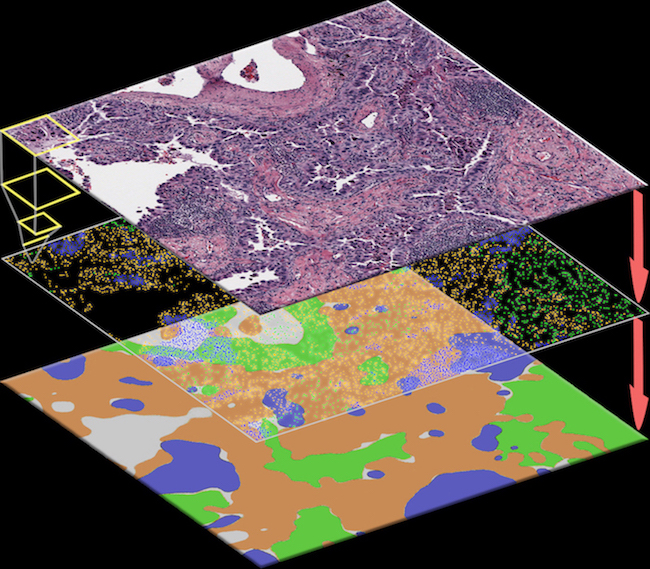
New software tool uses AI to help doctors identify cancer cells
UT Southwestern researchers have developed a software tool that uses artificial intelligence to recognize cancer cells from digital pathology images – giving clinicians a powerful way of predicting patient outcomes.
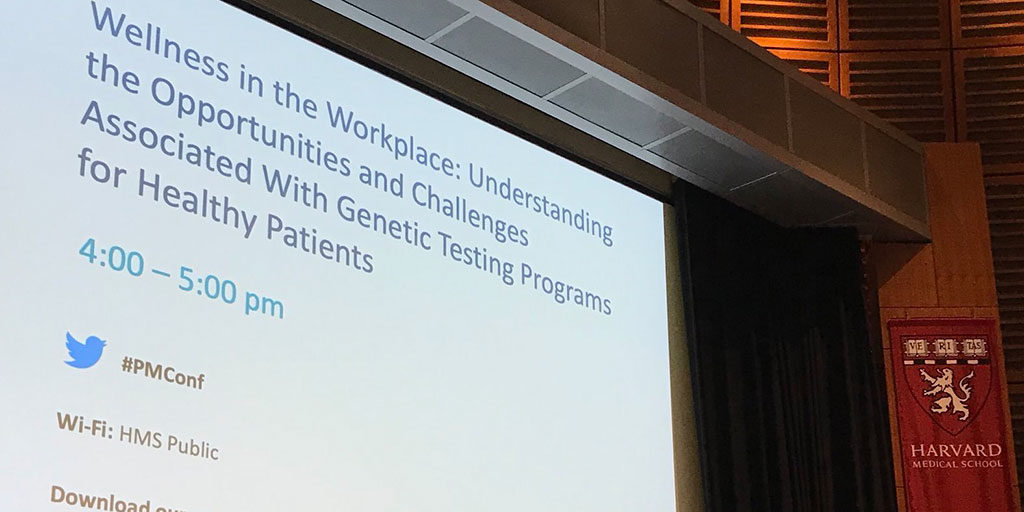
Science in Action: Wellness in the Workplace with Genetic Testing
The cost of genetic testing has steadily declined since the human genome was first mapped in 2003, allowing large employers, healthcare systems, and pension funds to adopt an upstream approach to preventative care by offering genetic testing and precision medicine as proactive wellness benefits.