Laboratory studies testing both methods in six models of breast cancer; five human cancer cell lines and one mouse cancer in mice with three variants of the immune system found that nanoparticles coated with trastuzumab, a drug that targets human epidermal growth factor receptor 2 (HER2)-positive breast cancer cells, were better retained in the tumors than plain nanoparticles, even in tumors that did not express the pro-growth HER2 protein. However, immune cells of the host exposed to nanoparticles induced an anti-cancer immune response by activating T cells that invaded and slowed tumor growth.
A description of the work will be published March 25 in Science Advances.
“It’s been known for a long time that nanoparticles, when injected into the bloodstream, are picked up by scavengerlike macrophages and other immune system cells,” explains senior study author Robert Ivkov, Ph.D., M.Sc., associate professor of radiation oncology and molecular radiation sciences at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins. “Many researchers in the field have been focused on trying to reduce interactions with immune cells, because they have been trying to increase the circulation time of the nanoparticles and their retention in tumor cells. But our study demonstrates that the immune cells in the tumor collect and react to the particles in such a way to stimulate an anti-cancer response. This may hold potential for advancing beyond drug delivery toward developing cancer immunotherapies.”
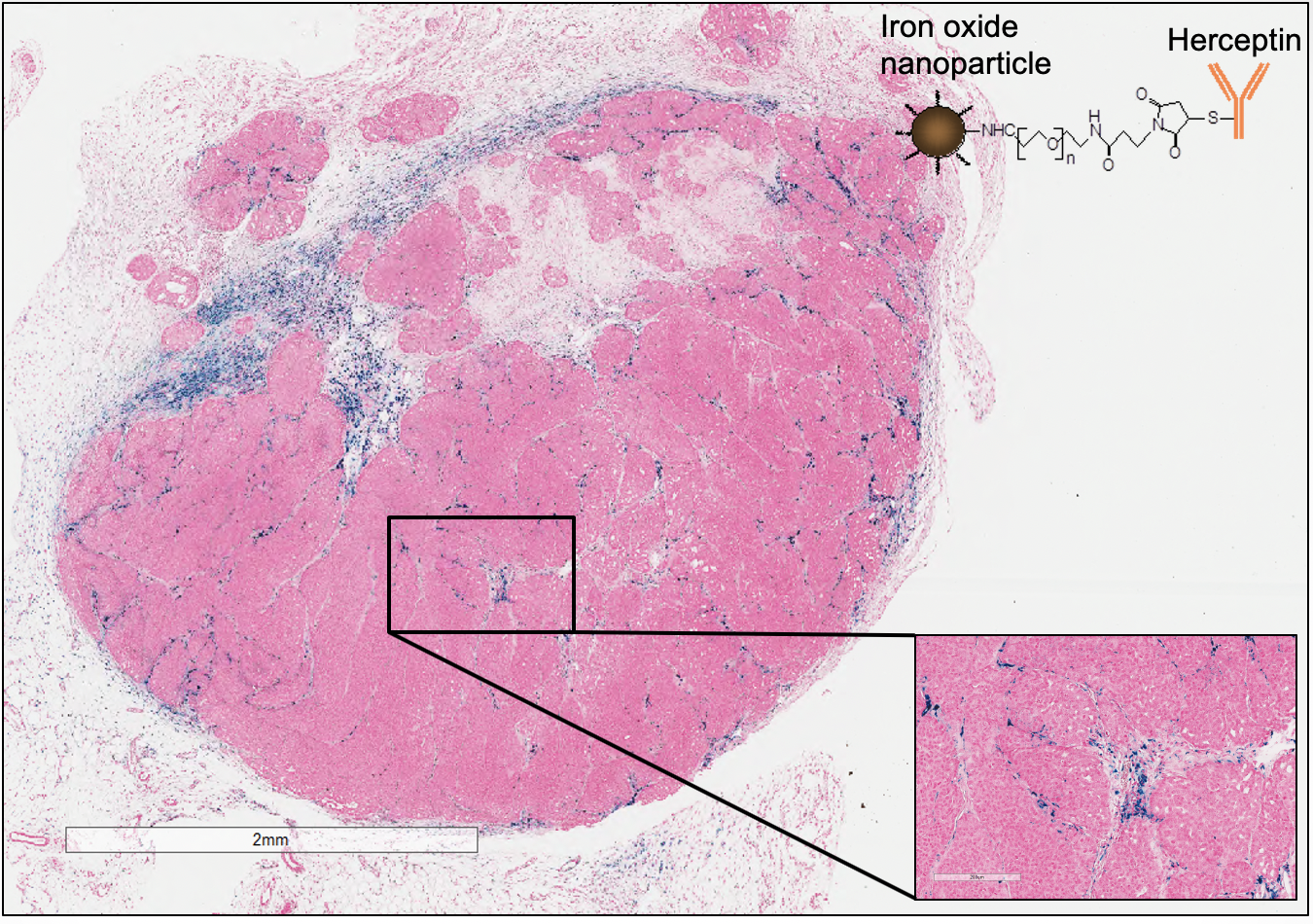
The investigators conducted a few in vitro experiments in their study. First, they applied some plain starch-coated iron oxide nanoparticles and others coated with trastuzumab to five human breast cancer cell lines, finding that the amount of binding between the trastuzumab-coated nanoparticles and cells depended on how much the cancer cells expressed the oncogene HER2. In people, HER2-positive breast cancers are among the most resistant to standard chemotherapy. Trastuzumab, sold under the name Herceptin, targets the HER2-positive tumor cells and triggers the immune system as well.
Responses were surprisingly different in animal models, the researchers report. In separate experiments, the team used the nanoparticles in two immune-deficient strains of mice engrafted with cells from five human breast cancer cell lines — two that were HER2 negative and three that were HER2 positive. When they studied the animals’ tumors 24 hours later, they noticed that nanoparticles coated with trastuzumab were found in a concentration two to five times greater than the plain nanoparticles in all types of tumors, regardless of whether they expressed the HER2 protein. They also found that the amount of trastuzumab-coated nanoparticles was even greater (tenfold) in mice that had a fully functional immune system and were bearing mouse-derived tumors.
This led the researchers to suspect that the host animals’ immune systems were interacting strongly with the nanoparticles and playing a role in determining retention of the particles in the tumor, whether or not a drug was added.
More experiments, the team reports, revealed that tumor-associated immune cells were responsible for collecting the nanoparticles, and that mice bred with an intact immune system retained more of the trastuzumab-coated nanoparticles than mice bred without a fully functioning immune system.
In addition, inflammatory immune cells in the tumors’ immediate surroundings, or microenvironment, seized more of the coated nanoparticles than the plain ones. Finally, in a series of 30-day experiments, the researchers found that exposure to nanoparticles inhibited tumor growth three to five times more than controls, and increased CD8-positive cancer-killing T cells in the tumors. Surprisingly, Ivkov notes, the anti-cancer immune activating response was equally effective with exposure to either plain or trastuzumab-coated nanoparticles. Mice with defective T cells did not show tumor growth inhibition. The investigators say this demonstrated that systemic exposure to nanoparticles can cause a systemic host immune response that leads to anti-cancer immune stimulation, and does not require nanoparticles to be inside the tumors.
“Overall, our work suggests that complex interdependencies exist between the host and tumor immune responses to nanoparticle exposure,” Ivkov says. “These results offer intriguing possibilities for exploring nanoparticle ‘targeting’ of the tumor immune microenvironment. They also demonstrate exciting new potential to develop nanoparticles as platforms for cancer immune therapies.”
The investigators say they also plan to study whether the same types of immune responses can be generated for noncancer conditions, such as infectious diseases.
Study coauthors were Preethi Korangath, James Barnett, Anirudh Sharma, Elizabeth Henderson, Jacqueline Stewart, Shu-Han Yu, Sri Kamal Kandala, Chun-Ting Yang, Julia Caserto, Mohammad Hedayati, Todd Armstrong, Elizabeth Jaffee, Xian Zhou, Wei Fu, Chen Hu, Saraswati Sukumar and Brian Simons of Johns Hopkins, and Cordula Grüttner of micromod Partikeltechnologie, GmbH, in Rostock, Germany.
The work was supported by the Jayne Koskinas Ted Giovanis Foundation for Health and Policy, and grants from the National Institutes of Health (#5R25GM109441) and the National Institutes of Health/National Cancer Institute (#P30 CA006973). Ivkov is an inventor on several issued and pending patents. All patents are assigned to The Johns Hopkins University or Aduro Biotech Inc. Grüttner is an employee of micromod Partikeltechnologie, GmbH, manufacturer of BNF nanoparticles used in the studies.
Original post https://alertarticles.info