In a developing embryo, both brain and immune system are not fully formed. The immune system, for its part, consists mostly of an “innate” system of cells that respond immediately to infection and do not require training or produce antibodies. Nevertheless, these cells require signals that prompt them to move toward an infection site and trigger a response.
The research team found that the brain appears to contribute to the signals that guide the nascent immune system. When brainless frog embryos were infected with E. coli, only about 16% of embryos survived, while the presence of a brain protected more than 50% from the infection. By following markers of immune cells, researchers confirmed that the effect is not due to the missing brain somehow hampering immune system development because the composition of the immune cells remained the same with or without a brain. Instead, they found that the effect was due to the brain sending signals to the immune cells to move toward the site of an infection.
“We found that macrophages –innate immune system cells that can swallow up bacteria and destroy them to reduce the burden of an infection do not migrate appropriately without the presence of the brain” said Michael Levin, Vannevar Bush Professor of Biology at Tufts University’s School or Arts and Sciences and Associate Faculty at Harvard’s Wyss Institute, director of the Allen Discovery Center at Tufts and corresponding author of the study. “Without the brain and its neurotransmitter signals, gene expression and innate immune system activity go awry, resulting in increased susceptibility to bacterial pathogens. ”
Other roles for the embryonic brain signaling during infection may include inducing cellular responses, for example preventing cell death or reducing inflammation, that help protect against the harmful effects of the infection.
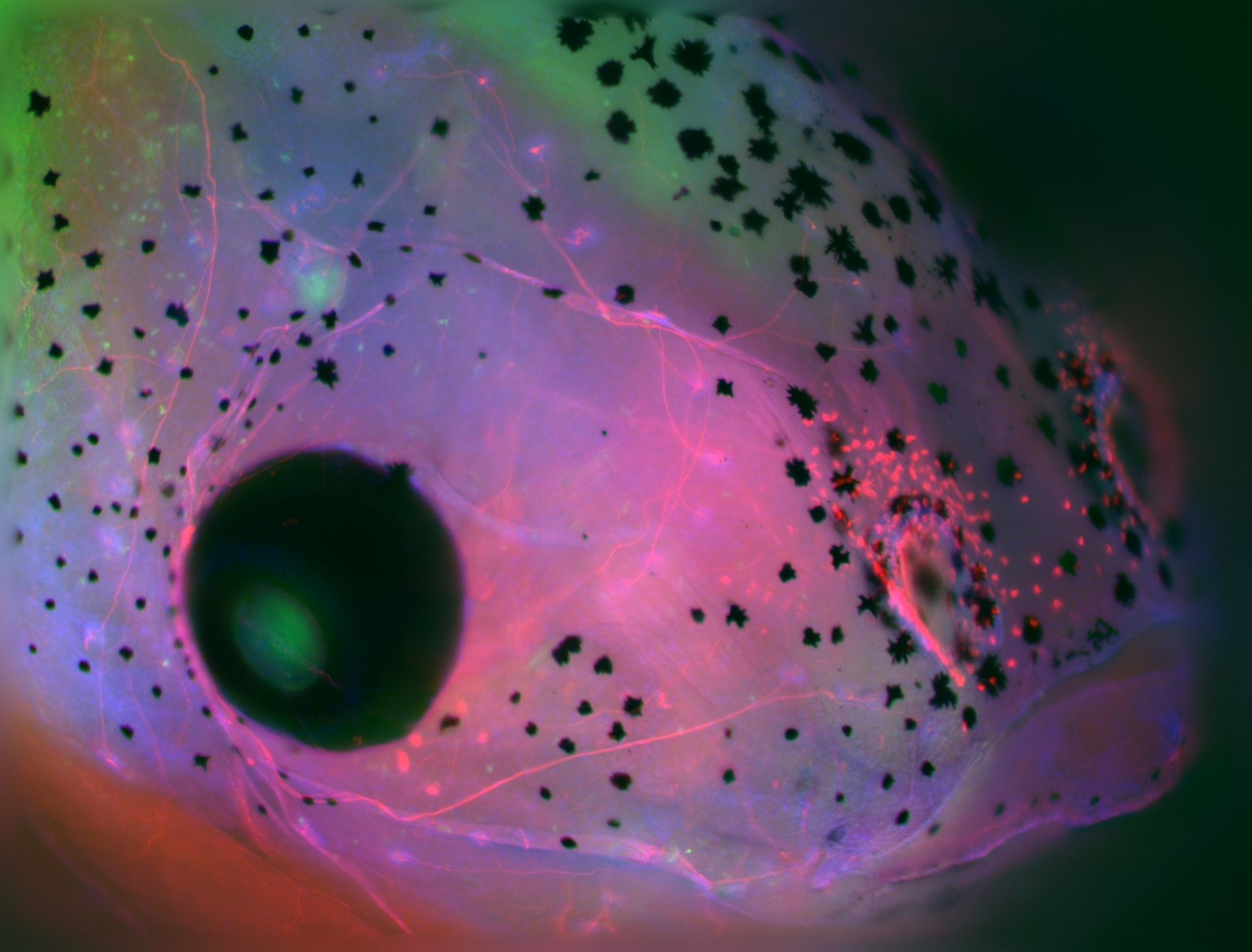
Immune system abberations were also observed in brainless embryos that were further developed. When the researchers tracked myeloid cells, a class of immune cells that includes macrophages, neutrophils and others, after an injury, they found that the myeloid cells in brainless embryos gathered in locations far from the injury site. By contrast, myeloid cells in normal embryos with intact brains would pile up at the injury site to assist in healing. In fact, in the brainless embryo, the myeloid cells tended to cluster around abnormal, disorganized peripheral nerve networks, also a by-product of brain absence, as demonstrated in earlier studies.
An examination of aberrations in genetic expression in brainless embryos also pointed to the reduction of the neurotransmitter dopamine (a signaling chemical used in the brain for learning and motivation), and that dopamine may play a role in activating immune cells to migrate in the early stages of an infection. The absence of an immune cell quorum at the infection site leads the brainless embryos to become more susectible to its lethal effects.
“Our results demonstrate the deep interconnections within the bacteria-brain-body axis: the early brain is able to ‘sense’ the pathogenic bacteria and to elaborate a response targeted to fight against the cellular and molecular consequences of the infection,” said Celia Herrera Rincon, Research Scientist II at the Allen Discovery Center at Tufts, and first author of the study.
Other authors of this study include: Jean-Francois Paré, Christina Harrison, Alina Fischer, and Sophia Jannetty at the Allen Discovery Center at Tufts; Christopher Martyniuk, associate professor in the Department of Physiological Sciences at University of Florida; and Alexandre Dinis and Vishal Keshari, graduate students, and Richard Novak, senior staff engineer at the Wyss Institute for Biologically Inspired Engineering, Harvard Universiy.
This research was supported by the Templeton World Charity Foundation Independent Research Fellowship (TWCF0241) and the Allen Discovery Center program through The Paul G. Allen Frontiers Group (12171), as well as The Defense Advanced Research Projects Agency (DARPA, W911NF-16-C-0050), and the National Institutes of Health (AR055993, AR061988). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Herrera-Rincon, C., Paré, J-F, Martyniuk, C.J., Jannetty, S.K., Harrison, C., Fischer, A., Dinis, A., Keshari, V., Novak, R., and Levin, M. “An in vivo brain–bacteria interface:the developing brain as a key regulator of innate immunity.” NPJ Regenerative Medicine (31 Jan 2020) DOI: 10.1038/s41536-020-0087-2
###
About Tufts University
Tufts University, located on campuses in Boston, Medford/Somerville and Grafton, Massachusetts, and in Talloires, France, is recognized among the premier research universities in the United States. Tufts enjoys a global reputation for academic excellence and for the preparation of students as leaders in a wide range of professions. A growing number of innovative teaching and research initiatives span all Tufts campuses, and collaboration among the faculty and students in the undergraduate, graduate and professional programs across the university’s schools is widely encouraged.
Original post https://alertarticles.info