They found that more than half—60%–of the counties with the highest death, or mortality, rates were in three states: Oklahoma, Texas, and New Mexico. Counties in Maryland, Nebraska and Pennsylvania had the lowest death rates from liver diseases.
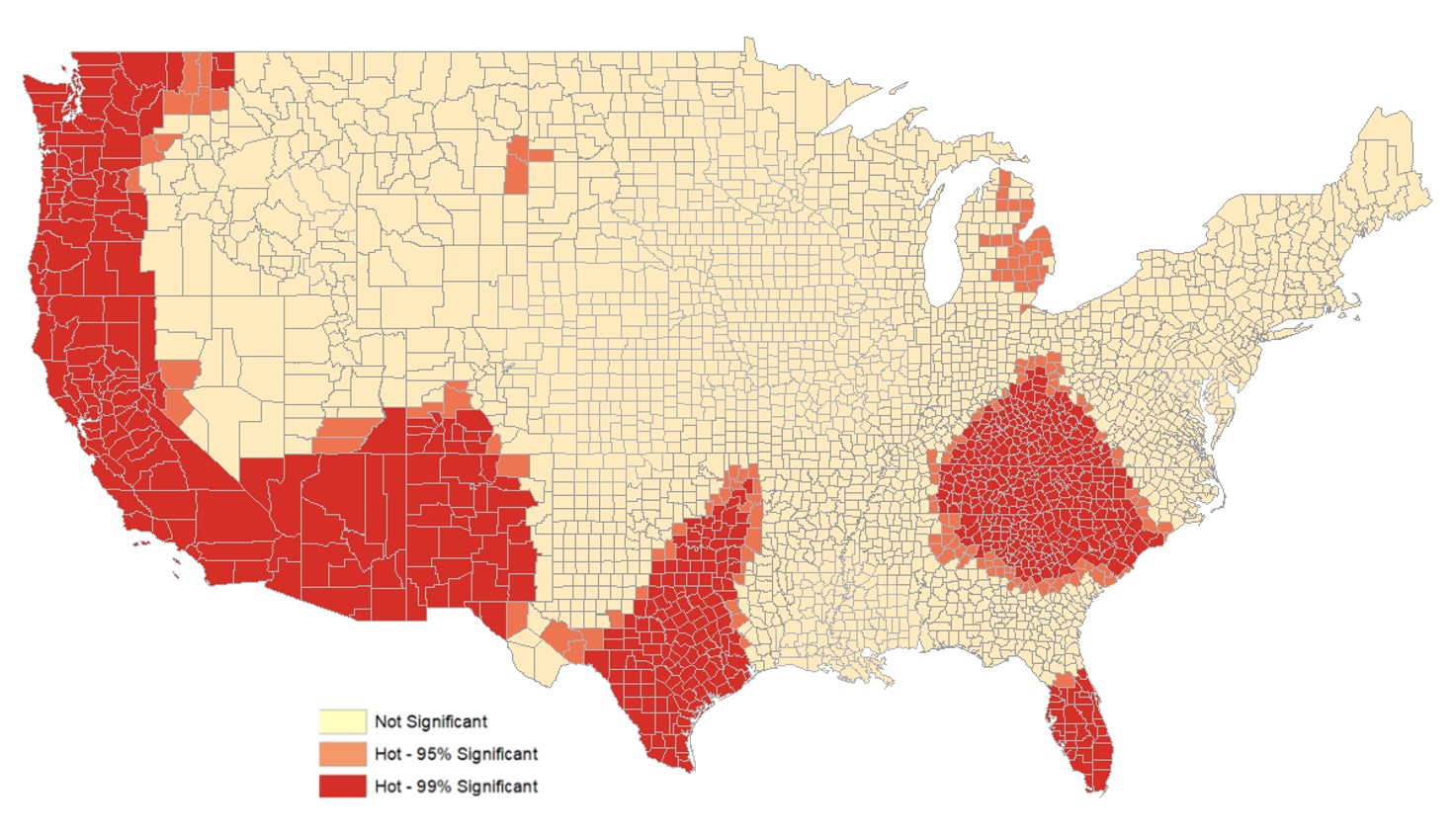
Interestingly, the researchers identified South Florida as the first of five clusters, or hotspots, for high liver disease mortality. The other four: Appalachia and the eastern part of the Midwest; Texas and Oklahoma; New Mexico, Arizona, California, and southern Oregon; and parts of Washington and Montana.
It is important to better understand factors contributing to what have become concerning trends in U.S. liver disease mortality. For example, annual deaths from cirrhosis spiked 65% and liver cancer mortality doubled between 1999 and 2016, according to prior studies.
“The most notable trends in liver-related mortality were increased rates among younger people (ages 25 to 34), whites, Native Americans, and Hispanics, and patients with alcohol-related liver disease,” the authors wrote.
But the available data prevented researchers from examining factors at the local level that could be contributing to the variability in death rates from liver disease across the U.S.
“We needed local or county level data to better explain why rates of death from liver disease, including liver cancer, were so high in some parts of the country and lower in others,” said the study’s first author David Goldberg, M.D., MSCE, associate professor of medicine, Division of Digestive Health and Liver Diseases at the Miller School.
Miller School and Emory University researchers collaborated to study CDC data from 2009-2018 on liver disease-related death rates.
They analyzed the data not only by county but also by hotspot, looking for clusters of excessively high liver disease mortality, even after adjusting for factors that might explain high rates, such as population composition and socioeconomic status. Counties that are a part of a hotspot might not have the highest mortality but are higher than statistically expected and are surrounded by other counties that are higher than expected.
“There is a large Hispanic population in South Florida. Another possible explanation is access to health care insurance is an issue in South Florida. Our study showed that counties with higher percentages of uninsured patients had higher liver disease-related mortality rates. There also are certain risk factors that may be higher in certain populations here, such as diabetes,” Dr. Goldberg said. “While this study does not fully explain why this and other areas are hot spots, we have identified potential county level factors. The next step is to look at individual patient factors that are associated with higher or lower rates of death from liver disease.”
Dr. Goldberg said many associate liver disease with alcoholism. In fact, today’s most common cause of liver disease is called non-alcoholic fatty liver disease, a metabolic liver disease that is more common in people who have diabetes and those who are overweight. Non-alcoholic fatty liver disease also is more common in certain populations, especially Hispanics.
There are policy initiatives that could help reduce mortality rates from liver disease, including more telehealth coverage and outreach geographically isolated patients; opening more liver transplant centers where they are most needed, based on this data; and addressing local needs to especially for populations with end-stage liver disease.
“At a time when expansion of the Affordable Care Act remains a controversial political issue, these data show some of the potential consequences of not providing insurance access at the county level,” he said.
Coauthors on the paper are Katherine Ross, M.P.H., Ph.D. student in epidemiology, Rollins School of Public Health, Emory University, and Raymond Lynch, M.D., a transplant surgeon at Emory University.