As a scientist, she was fascinated by the capricious nature of the disease as it severely affected certain healthy individuals while paradoxically sparing other people, including some with weakened immune systems. “I was hooked,” she confessed. As a physician, she was deeply moved by stories about some young people perishing from the new illness after initially seeming to recover. She soon reached out to a colleague in the Smidt Heart Institute at Cedars-Sinai.
“You go into medicine and research to make a difference,” said Cheng, director of Public Health Research at the institute. “My colleague and I both said we had to do something about this. We then shifted everything we were doing to focus on COVID-19 research.”
Making Major Discoveries
As Cheng pivoted, so did the research enterprise at Cedars-Sinai and its hundreds of medical investigators. Scientists specializing in cardiology, pulmonology, gastroenterology, genetics, cancer and other fields set aside their own research priorities and turned their attention to COVID-19.
A year into the pandemic, they have launched more than 100 studies, including more than 20 clinical trials, involving SARS-CoV-2, the novel coronavirus that causes COVID-19, and published game-changing discoveries in the world’s top-tier journals, including The New England Journal of Medicine and the Journal of the American Medical Association.
Cedars-Sinai investigators uncovered a Southern California strain of the coronavirus and tracked its explosive spread. They participated in pioneering clinical trials that would add the therapies remdesivir and monoclonal antibodies to the arsenal of treatments for the disease. They forged a powerful COVID-19 research consortium across multiple U.S. institutions, igniting numerous studies involving thousands of healthcare workers and patients. And they established Cedars-Sinai as a center for the National Cancer Institute’s drive to understand and control the spread of COVID-19, focusing on the pandemic’s unequal impact on racial and ethnic groups.
Collaborating With Clinicians
To manage the multitude of evolving projects, Cedars-Sinai’s research leaders invented new ways of working and refocused their research virtually overnight. They formed a COVID-19 Research Task Force of clinicians and scientists to help oversee coronavirus studies and accelerate research collaborations across the institution. They scheduled virtual “journal clubs” to present the latest findings and studies-in-process.
And especially in the pandemic’s early days, they rallied to help frontline workers cope with a crush of COVID-19 patients.
“We scoured our laboratories to find spare cotton swabs and reagents for the COVID-19 diagnostic tests, and we sent over protective masks,” said task force leader Clive Svendsen, PhD, professor of Biomedical Sciences and Medicine and executive director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute. “We manufactured gallons of hand sanitizer when the hospital began running out. We put everything into a special COVID-19 storage room.”
The Department of Pathology and Laboratory Medicine, while developing an entirely new COVID-19 testing facility for clinical use, also co-led a Cedars-Sinai study that traced most early cases in Southern California to a virus version from New York state via Europe, not directly from China.
Research labs repurposed several of their ultra-cold freezers, normally used to store tissue samples and cells for studies, to the Pharmacy Department. This transfer also enabled Cedars-Sinai in December to be among the first hospitals in the country to receive shipments of the Pfizer-BioNTech vaccine, which must be housed at -80 degrees Celsius.
“Cedars-Sinai’s rapid response to the COVID-19 pandemic benefited tremendously from the seamless synergy of our academic and clinical operations,” said Shlomo Melmed, MB, ChB, executive vice president of Academic Affairs and dean of the medical faculty. “The challenge inspired our investigators to make discoveries that ease human suffering and save lives. The pandemic has lent new urgency to this important mission at Cedars-Sinai and throughout the medical science world.”
Testing a Promising Treatment
From the first months of the pandemic, Cedars-Sinai scientists made critical contributions to understanding the puzzling disease.
Thirteen Cedars-Sinai staff members, including Jonathan Grein, MD, director of Hospital Epidemiology, contributed to an early case series by the Centers for Disease Control and Prevention (CDC) that identified the most common symptoms of coronavirus infections. The findings were reported in Nature Medicine, a leading peer-reviewed journal.
Grein also co-authored a study in The New England Journal of Medicine that reported clinical improvement in COVID-19 patients treated with the antiviral drug remdesivir. “We look forward to the results of controlled clinical trials to validate these findings,” Grein said then.
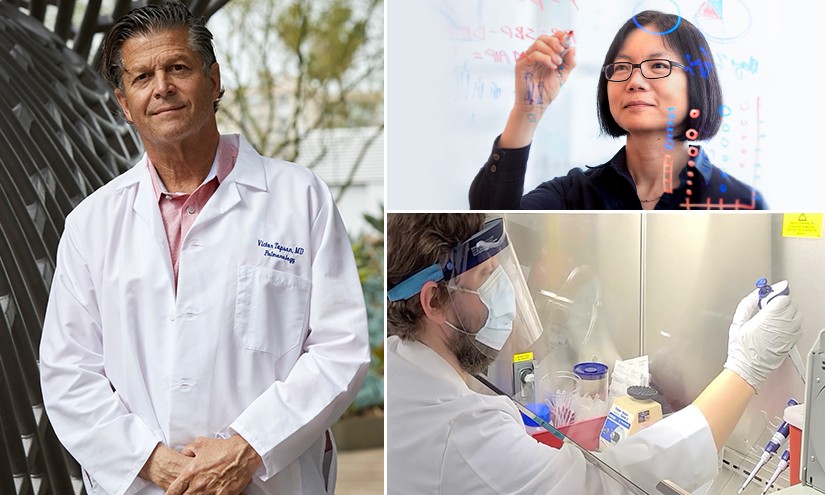
Grein’s colleague Victor Tapson, MD, along with investigators at dozens of sites around the world, had already started to make that happen. He enrolled Cedars-Sinai patients in the first randomized, controlled clinical trial of remdesivir sponsored by the National Institutes of Health. Tapson, clinical research director at the Women’s Guild Lung Institute at Cedars-Sinai, would later co-author an article in The New England Journal of Medicine reporting their findings.
All these efforts paid off for patients and doctors everywhere when remdesivir became the first drug to receive emergency use authorization from the Food and Drug Administration for people hospitalized with COVID-19 and later won approval as a treatment. Remdesivir remains the only FDA-approved therapy for COVID-19.
“It is truly gratifying that Cedars-Sinai has played such a significant role in making an important drug available to those in need,” said Tapson, who recently co-authored another article in The New England Journal of Medicine reporting on a successor COVID-19 trial combining remdesivir and the anti-inflammatory drug baricitinib.
Tracking Down a New Strain
In late December 2020, Wenjuan Zhang, PhD, assistant professor of Pathology and Laboratory Medicine at Cedars-Sinai, began hunting for a coronavirus variant called B.1.1.7, which was first identified in the UK. She worried that the variant, believed to be more contagious, would turn up in local virus samples. It did not.
Surprisingly, she made a troubling discovery: A new version of the virus was rapidly spreading among COVID-19 patients in Southern California and beyond. Zhang and colleagues named the version CAL.20C and published their findings in the Journal of the American Medical Association (JAMA), attracting the attention of Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and the Biden administration’s chief medical adviser, who wrote a commentary pointing to the public health importance of these findings.
Since then, the CAL.20C strain (also known as B.1.427/ B.1.429) has continued to spread around the country and the world. By February, it accounted for more than half the cases in California and nearly as many in Nevada. According to the CDC, this variant, which earlier this month was catalogued as a “variant of concern,” alongside B.1.1.7 and two more variants, shows signs of possibly being more transmissible, resistant to treatment or otherwise posing a higher clinical risk.
Now researchers are on an urgent quest to learn whether CAL.20C is indeed more dangerous.
“We are expanding our clinical database so that we can determine if CAL.20C has a distinctive impact on patient outcomes,” said Jasmine Plummer, PhD, a research scientist at the Cedars-Sinai Center for Bioinformatics and Functional Genomics and co-senior author of the JAMA paper, along with Eric Vail, MD, assistant professor of Pathology and Laboratory Medicine.
“Is COVID-19 worse if the patient is infected with the CAL.20C variant, and does it present with different symptoms?” Plummer said. “These questions are critical to understanding and defeating this disease.”
Rallying Other Institutions
At the heart institute a year ago, Cheng realized that pushing the pace of pandemic research would require a rapid-response team of clinician-scientists, epidemiologists, pathologists, immunologists, analytical chemists and biostatisticians, both inside and outside Cedars-Sinai. And there was no time to waste.
“So at my kitchen table, I created the CORALE website,” recalled Cheng, associate professor of Cardiology. CORALE, which stands for Coronavirus Risk Associations and Longitudinal Evaluation study, is a research network with experts from multiple California institutions, including Cedars-Sinai, and Brigham and Women’s Hospital in Boston.
CORALE’s ambitious goal is “to generate new knowledge to inform public health efforts aimed at reducing overall risks from the SARS-CoV-2 virus and similar viruses in the future.”
The network is well on its way to meeting that goal, publishing more than a dozen studies over the last year. Many focus on showing how the virus affects different populations based on gender, race, ethnicity and preexisting conditions.
One study found that healthcare workers are more likely to have antibodies to COVID-19 in their blood if they are African American or Latinx and that the community—rather than the workplace—appeared likely to be the more common source of coronavirus exposure. This research leveraged data from more than 6,000 Cedars-Sinai employees who volunteered to fill out surveys and take blood tests.
CORALE’s concerted efforts were essential for winning a five-year, $8.3 million grant from the National Cancer Institute (NCI) to Cedars-Sinai to study the diversity and determinants of the immune-inflammatory response to SARS-CoV-2. Cedars-Sinai is one of just eight centers for the NCI’s Serological Sciences Network, or SeroNet, initiative to deploy serological testing to the American public, improve understanding of the immune response to SARS-CoV-2 and help control the spread of the virus.
An important study posted on MedRxiv from CORALE demonstrated that individuals who previously had COVID-19 generated an immunologic response after a single dose of the Pfizer-BioNTech vaccine that was similar to individuals receiving the two-dose recommended sequence. If confirmed, a single-dose strategy for those who previously had COVID-19 could save millions of vaccine doses to be deployed elsewhere.
What’s next for Cheng’s team and CORALE? “We’re looking into post-COVID syndromes,” Cheng said. “The nature of how this virus affects some people more than others is still very mysterious—not only regarding acute infection but now also the after-effects, the so-called long-haulers. Ultimately, we want to learn how to be better prepared for the next pandemic.”
Advancing on Many Fronts
Cedars-Sinai investigators made many other discoveries in the past year that shed significant light on the pandemic. Among them:
- Peter Chen, MD, professor of Medicine and director of the Division of Pulmonary and Critical Care Medicine, was first co-author of a multisite clinical trial, published in The New England Journal of Medicine, testing the monoclonal antibody LY-CoV555 as a potential COVID-19 treatment. He and colleagues also published a study in the journal Cell Reports that revealed immune system malfunctions in COVID-19 patients who develop respiratory failure.
- Moshe Arditi, MD, professor of Pediatrics and Biomedical Sciences and director of the Pediatric and Infectious Diseases and Immunology Division, was co-senior author of a study in The Journal of Clinical Investigation showing that a widely used tuberculosis vaccine known as Bacillus Calmette-Guérin (BCG) was associated with reduced likelihood of contracting COVID-19.
- Raj Makkar, MD, professor of Medicine at the heart institute, led what was believed to be the first peer-reviewed report on using a cell therapy in critically ill COVID-19 patients. The therapeutic, known as CAP-1002, contains cardiosphere-derived cells (CDCs) that are grown in the laboratory from human heart tissues.
- Clive Svendsen, PhD, and Arun Sharma, PhD, a research fellow at the Regenerative Medicine Institute, were co-corresponding authors of a Cell Reports Medicine study showing that SARS-CoV-2 can infect heart cells in a lab dish. The discovery was made using heart muscle cells that were produced by stem cell technology.
Looking ahead, Jeffrey A. Golden, MD, vice dean for Research and Graduate Research Education and director of the Burns and Allen Research Institute at Cedars-Sinai, anticipates many additional scientific advances in the war against the coronavirus.
“More importantly, we have learned over the past year that by working together, the extraordinary and collaborative investigators at Cedars-Sinai can achieve remarkable advances to confront any adversity,” he said. “Furthermore, we do so thinking about our four core missions: providing world-class clinical care to our patients, advancing our understanding of disease to help our patients and those everywhere, educating the next generation, and supporting the many communities we serve.”
Read more about how Cedars-Sinai research is helping COVID-19 patients in Discoveries: Model Predicts How Many COVID-19 Patients Will Need Care
About #YearofCOVID
One year has passed since stay-at-home orders went into effect across the U.S. and the COVID-19 pandemic changed our lives in profound ways. The novel coronavirus has infected hundreds of millions worldwide and killed millions, including more than 500,000 in the U.S alone. It has separated many from their loved ones and cost others their jobs, their homes and their life savings.
But in a dark year, we’ve also witnessed courageous patients and heroic healthcare workers battling the disease, as swift scientific breakthroughs have brought us vaccines and hope.
During March, the Cedars-Sinai Newsroom team is marking this one-year pandemic milestone with a series reflecting on the past 12 months as experienced by our patients, healthcare workers, researchers and community. Follow and join the conversation on social media @CedarsSinai.