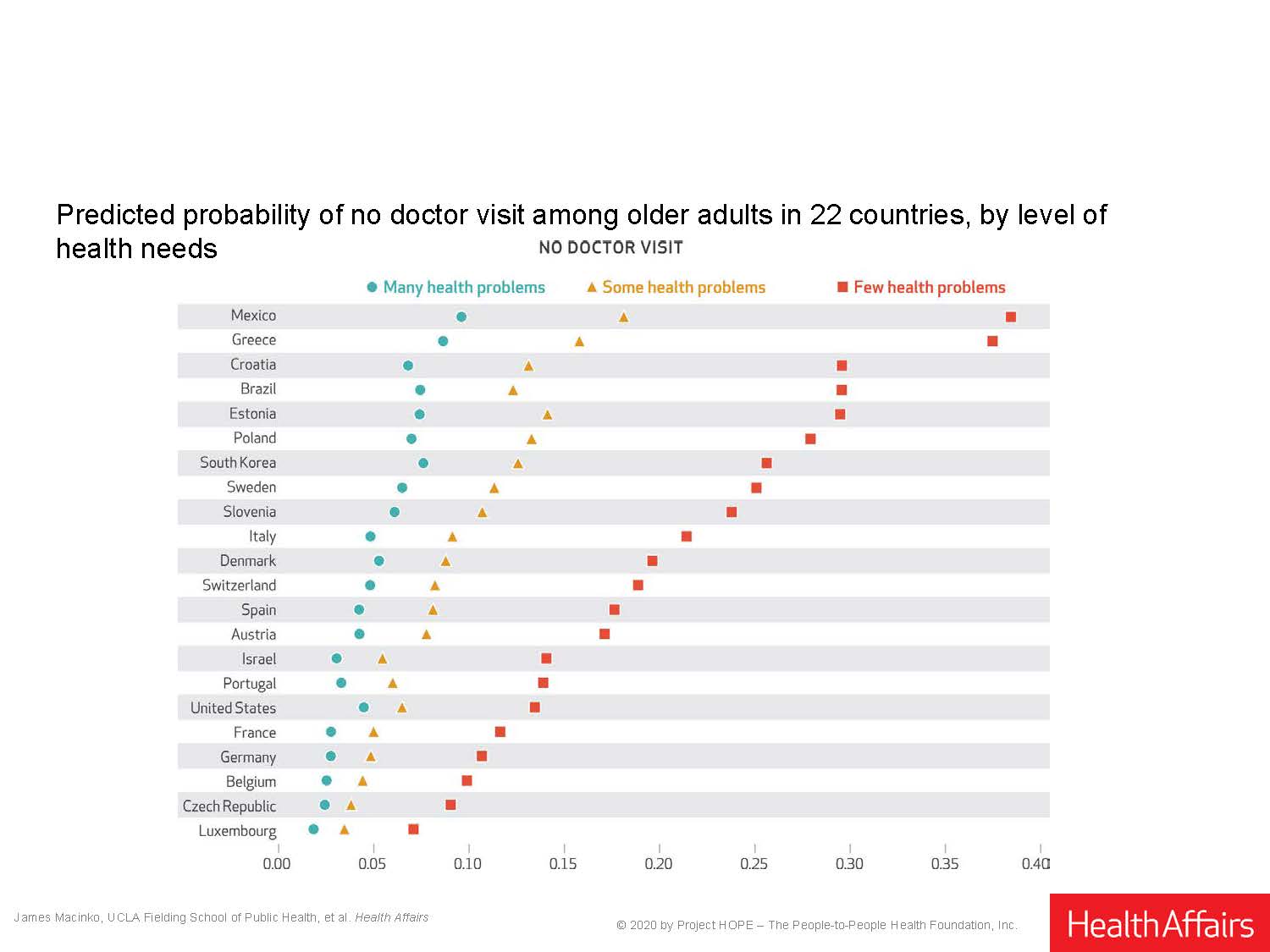
In terms of best practices, such as an annual doctor’s check-up, the U.S. came in at 7th place, with almost 8.5% of the over-50 population not seeing a doctor in 2016, the year that was surveyed. By contrast, a significantly higher percentage of older people in the Czech Republic, Belgium, France, Germany, Luxembourg, and Portugal than Americans got to see a doctor, with the shortfall ranging from roughly 5% in the Czech Republic to 7% in France.
“In the highest-performing health systems such as those of the richer countries of Western Europe, older adults almost all were able to consult a doctor, at least annually, without incurring high out of pocket expenses,” said James Macinko, UCLA Fielding School of Public Health professor in the departments of Community Health Sciences and Health Policy and Management. “That is not as common an outcome in the U.S.”
The study was published in the November edition of the peer-reviewed journal Health Affairs, and includes authors from universities in the U.S. and Brazil. The researchers’ work examined some 100,000 older adults in one of the largest studies ever investigating cross-national differences in health care access, use, and related health expenditures among older adults, and one of only a handful that has investigated health system factors.
The countries surveyed include the U.S. and several with comparably high per capita incomes, including Luxembourg, Switzerland, Denmark, Sweden, Austria, Germany, and France, most of which have some variant of universal health coverage.
Not all the team’s findings reflected poorly on the U.S. system, especially when it came to access to doctor visits. The access to care provided by the U.S. healthcare system comes with a price, however, researchers found. When it came to “catastrophic healthcare expenditures” (defined as when 25% or more of household income had to be spent out of pocket on health care), the U.S. ranked last in terms of high-income countries, although higher rates were observed in Eastern European and middle-income countries such as Brazil and Mexico.
“Even though catastrophic expenses in the U.S. are higher than in other comparable high-income countries, they affect only about 3% of the U.S. population aged 50 and over,” said study co-author Flavia Cristina Drumond Andrade, an associate professor in the School of Social Work at the University of Illinois. “This is perhaps as a result of higher average income levels and the fact that in the U.S., adults ages 65 and older have access to a national health insurance program (Medicare), and additional coverage options are available to help defray costs through Medigap, employer-sponsored insurance, or Medicaid.”
The researchers found that after individual characteristics and health needs were controlled for, national rates varied up to tenfold for poor access (no doctor visit) and threefold for potential overutilization (15 or more doctor visits and multiple hospitalizations) in the past year.
In terms of hospitalization, the U.S. had the highest number of older patients hospitalized, with more than 9 percent hospitalized two or more times in the past year, as opposed to as few as 6.5 percent in Germany, 5.5 percent in France, roughly 5 percent in Sweden and Switzerland, and a little over 4 percent in Denmark. A significant proportion of these events are re-hospitalizations that occur due to poor quality or inadequate follow-up care.
“Access to care remains a problem for 11 percent of all adults examined here, and in six countries, this figure reached or exceeded 15 percent,” Macinko said. “There are numerous ways to enhance access, and all of these approaches may also strengthen the primary care basis of health systems such as using telemedicine for remote consultation and triage, employing community health workers for home care and control of some chronic disease risks, and guaranteeing access after-hours and on weekends to avoid relying on urgent care or hospital emergency departments, and these approaches could further enhance access, improve care coordination and integration for chronic conditions, and help contain health care expenditure growth.”
Funding: Although the individual studies included in the analysis were funded by the NIH, among other agencies, no specific source funded this analysis.
Data Availability Statement: All survey data are publicly available through the websites of each country’s aging cohort survey. More information available in the publication.
Image Caption: Health care use and expenditure indicators (unadjusted) among older adults in 23 countries, ranked.
Image Credit: Authors’ analysis of data from aging cohort studies in twenty-three countries, 2014–16.
Citation: Macinko, James, (2020) Universal Health Coverage: Are Older Adults Being Left Behind? Evidence From Aging Cohorts In 23 Countries, Health Affairs 39, NO. 11 (2020): 1951–1960.
The UCLA Fielding School of Public Health, founded in 1961, is dedicated to enhancing the public’s health by conducting innovative research, training future leaders and health professionals from diverse backgrounds, translating research into policy and practice, and serving our local communities and the communities of the nation and the world. The school has 690 students from 25 nations engaged in carrying out the vision of building healthy futures in greater Los Angeles, California, the nation and the world.