The study was conducted by a team of scientists at UPMC Hillman Cancer Center and the University of Pittsburgh School of Medicine, led by Greg Delgoffe, Ph.D., Pitt associate professor of immunology. By disrupting the effect of the tumor microenvironment on immune cells in mice, the researchers were able to shrink tumors, prolong survival and increase sensitivity to immunotherapy.
“The majority of people don’t respond to immunotherapy,” said Delgoffe. “The reason is that we don’t really understand how the immune system is regulated within this altered tumor microenvironment.”
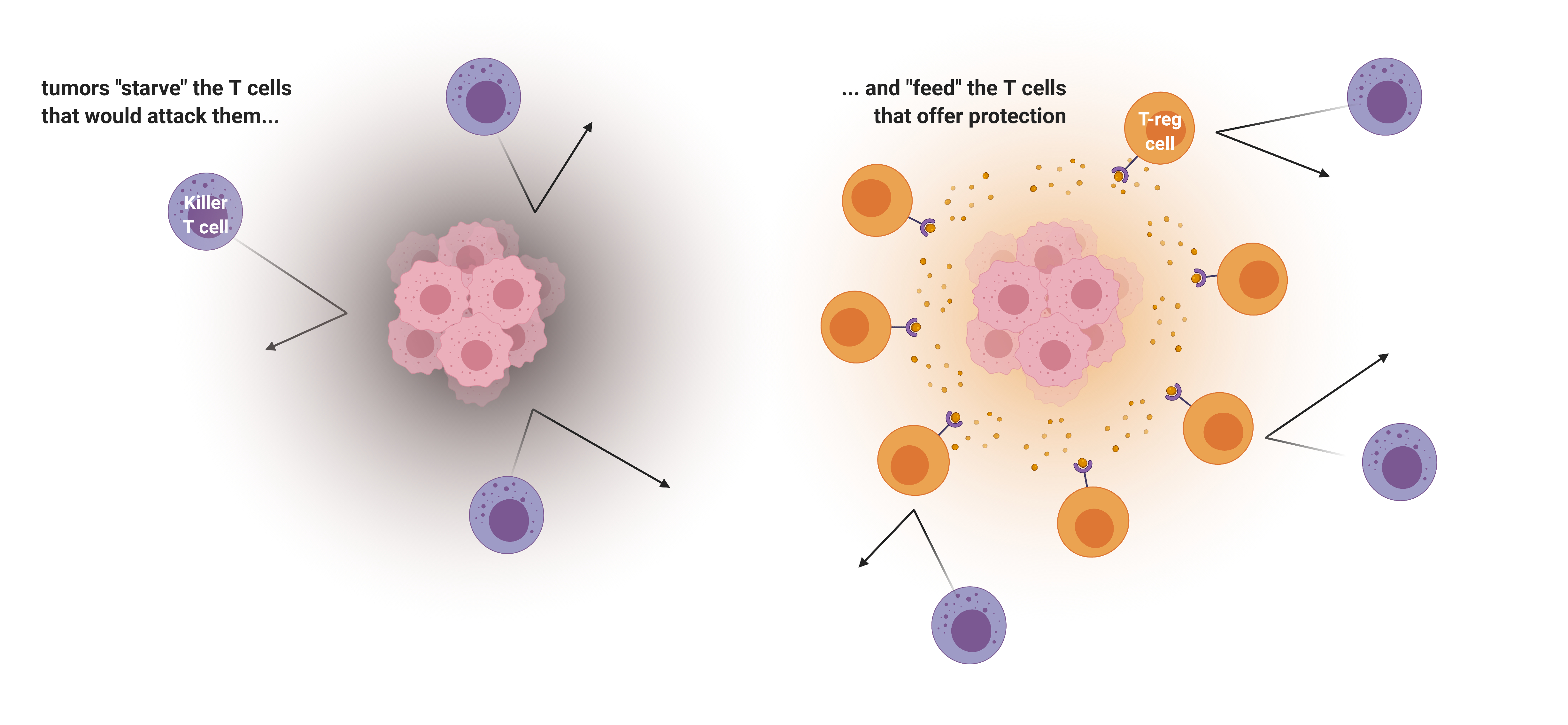
The immune system is made up of many kinds of cells, chief among them T cells. One type, called killer T cells, fights off invaders, such as viruses, bacteria and even cancer. Another type, called regulatory T cells, or “T-reg cells” for short, counteracts killer T cells by acting as protectors of the cells that belong to the body. T-reg cells are important for preventing autoimmune diseases, such as type I diabetes, Crohn’s disease and multiple sclerosis, where overactive killer T cells assault the body’s healthy tissues.
For all of these different immune cells to do their jobs, they need to produce energy. Delgoffe’s team studied how these different types of T cells have different appetites, and how tumors—which have large appetites—compete for nutrients with infiltrating immune cells. The researchers found that killer T cells and regulatory T cells have very different appetites, and cancer cells exploit this.
“Cancer is wise to the whole situation,” Delgoffe said. “Cancer cells don’t just starve T cells that would kill them but actually feed these regulatory T cells that would protect them.”
In short, Delgoffe’s team found that tumors gobble up all the vital nutrients in their vicinity that killer T cells would need to attack. Further, they also excrete lactic acid, which feeds the regulatory T cells, convincing them to stand guard. T-regs can turn the lactic acid into energy, using a protein called MCT1, so nuzzling up with the tumor is a good way for these immune cells to stay fed.
“What better way to recruit a cell than food?” Delgoffe said.
Then, using mice with melanoma, the researchers found that silencing the gene that codes for the MCT1 protein caused tumor growth to slow down. The mice also lived longer.
“We starved the T-regs,” said Delgoffe. “When T-reg cells are not being sustained by the tumor, killer T cells can come in and kill the cancer.”
Importantly, when Delgoffe’s team combined MCT1 inhibition with immunotherapy, the anti-cancer effects were stronger than either strategy alone.
Clinically, the same effect might be achievable using drugs that inhibit MCT1—one of which is currently being tested in people with advanced lymphoma, and it appears to be well-tolerated.
Additional authors on the study include McLane Watson, Paolo Vignali, Steven Mullett, Abigail Overacre-Delgoffe, Ph.D., Ronal Peralta, Stephanie Grebinoski, Ashley Menk, Natalie Rittenhouse, Kristin DePeaux, Ryan Whetstone, Ph.D., Dario Vignali, Ph.D., Timothy Hand, Ph.D., Amanda Poholek, Ph.D., and Stacy Wendell, Ph.D., of Pitt and UPMC; and Brett Morrison, M.D., Ph.D., and Jeffrey Rothstein, M.D., Ph.D., of Johns Hopkins University.
Funding for this study was provided by the Sidney Kimmel Foundation, National Institutes of Health (DP2AI136598, P50CA121973, P50CA097190 R01DK089125, R01CA203689, P01AI108545, T32CA082084, F31AI149971, F30CA247034, F31CA247129, T32AI089443 and F31AI147638), the American Association for Cancer Research (SU2CAACR-IRG-04-16), the Alliance for Cancer Gene Therapy, the Mark Foundation for Cancer Research, Cancer Research Institute, the Sy Holzer Endowed Immunotherapy Fund and the Damon Runyon Cancer Research Foundation.