The gene, Foxp1, has previously been studied for its function in the neurons of the developing brain. But the new study reveals that it’s also important in a group of brain stem cells — the precursors to mature neurons.
“This discovery really broadens the scope of where we think Foxp1 is important,” said Bennett Novitch, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA and the senior author of the paper. “And this gives us an expanded way of thinking about how its mutation affects patients.”
Mutations in Foxp1 were first identified in patients with autism and language impairments more than a decade ago. During embryonic development, the protein plays a broad role in controlling the activity of many other genes related to blood, lung, heart, brain and spinal cord development. To study how Foxp1 mutations might cause autism, researchers have typically analyzed its role in the brain’s neurons.
“Almost all of the attention has been placed on the expression of Foxp1 in neurons that are already formed,” said Novitch, a UCLA professor of neurobiology who holds the Ethel Scheibel Chair in Neuroscience.
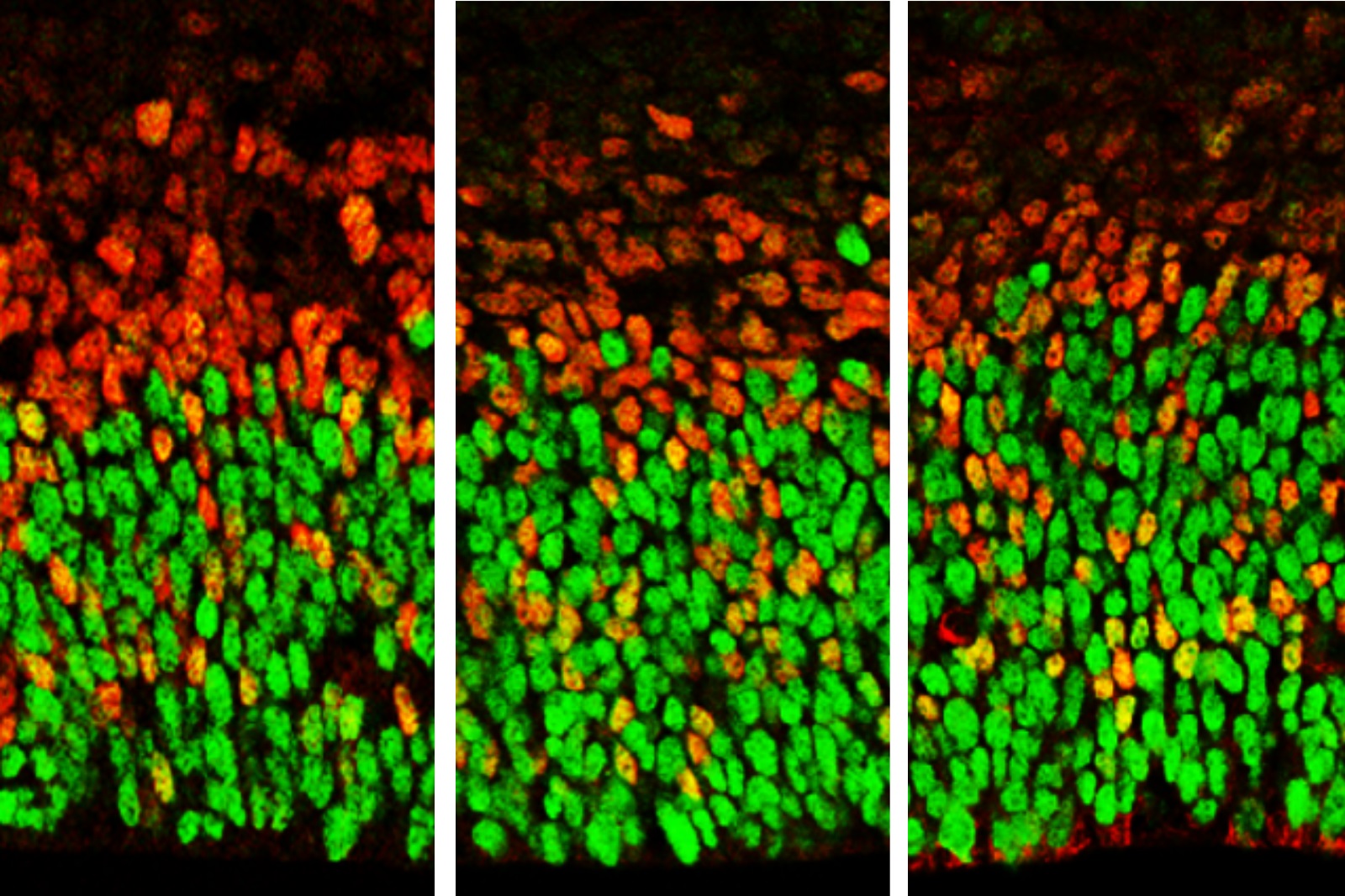
In the new study published in Cell Reports, he and his colleagues monitored levels of Foxp1 in the brains of developing mouse embryos. They found that, in normally developing animals, the gene was active far earlier than previous studies have indicated — during the period when neural stem cells known as apical radial glia were just beginning to expand in numbers and generate a subset of brain cells found deep within the developing brain.
When mice lacked Foxp1, however, there were fewer apical radial glia at early stages of brain development, as well as fewer of the deep brain cells they normally produce. When levels of Foxp1 were above normal, the researchers observed more apical radial glia and an excess of those deep brain cells that appear early in development. In addition, continued high levels of Foxp1 at later stages of embryonic development led to unusual patterns of apical radial glia production of deep-layer neurons even after the mice were born.
“What we saw was that both too much and too little Foxp1 affects the ability of neural stem cells to replicate and form certain neurons in a specific sequence in mice,” Novitch said. “And this fits with the structural and behavioral abnormalities that have been seen in human patients.”
Some people, he explained, have mutations in the Foxp1 gene that blunt the activity of the Foxp1 protein, while others have mutations that change the protein’s structure or make it hyperactive.
The team also found intriguing hints that Foxp1 might be important for a property specific to the developing human brain. The researchers also examined human brain tissue and discovered that Foxp1 is present not only in apical radial glia, as was seen in mice, but also in a second group of neural stem cells called basal radial glia.
Basal radial glia are abundant in the developing human brain, but absent or sparse in the brains of many other animals, including mice. However, when Novitch’s team elevated Foxp1 function in the brains of mice, cells resembling basal radial glia were formed. Scientists have hypothesized that basal radial glia also are connected to the size of the human brain cortex: Their presence in large quantities in the human brain may help explain why it is disproportionately larger than those of other animals.
Novitch said that although the new research does not have any immediate implications for the treatment of autism or other diseases associated with Foxp1 mutations, it does help researchers understand the underlying causes of those disorders.
In future research, Novitch and his colleagues are planning to study what genes Foxp1 regulates in apical radial glia and basal radial glia, and what roles those genes play in the developing brain.
The study’s first author is Caroline Alayne Pearson, a UCLA assistant project scientist. Other authors are from the University of Texas at Austin, the University of Alabama at Birmingham and the University of Puerto Rico.
The study was funded by the National Institutes of Health, the California Institute for Regenerative Medicine, the Cancer Prevention and Research Institute of Texas, the University of Texas at Austin’s Marie Betzner Morrow Centennial Endowment and the UCLA Broad Stem Cell Research Center’s Research Award Program, including support from the Binder Foundation.
Original post https://alertarticles.info