Led by the University of Washington (UW) School of Medicine in Seattle, CODA is a randomized clinical trial being conducted at 25 U.S. medical centers in 1,552 adults with appendicitis to discover if antibiotic treatment is as good as appendectomy. In results released early because of physicians’ interest, the researchers found that overall, the health of patients receiving antibiotic therapy was no worse a month later than that of patients who had their appendix removed.
“For the first time, these results will inform the typical appendicitis patients in the U.S. practice what the options are and what the expected results are for patients like them,” said study co-principal investigator David R. Flum, MD, MPH, FACS, professor and associate chair of surgery at UW School of Medicine. David Talan, MD, emergency medicine physician, Geffen School of Medicine at UCLA, is also co-principal investigator.
Dr. Flum said he expects the CODA results to greatly change appendicitis treatment in the United States. “Antibiotic treatment will be good for many people but not for all,” he explained.
Appendectomy has been the standard treatment of appendicitis for more than 120 years and is the most common emergency abdominal procedure performed in the United States.2 Despite evidence from European studies over the past 25 years that antibiotics successfully treat most patients with appendicitis,3 a recent study finds less than 5 percent of all U.S. patients with appendicitis receive nonoperative treatment.4
How CODA was unique
Dr. Flum said some U.S. doctors believed the European studies had shortcomings, which CODA, with the input of patient advisors, was designed to address. The new trial is answering patient-centered questions that, according to Dr. Flum, went unanswered in the European studies. These include whether initial treatment with antibiotics affects time away from work and in the hospital.
Also, he said the CODA patient population better represents typical U.S. surgical practices. The study includes patients with a broad range of appendicitis severity and those with an appendicolith, a small stone at the base of the appendix. Of CODA participants, 27 percent had an appendicolith on imaging, but the European studies excluded such patients because an appendicolith may indicate more complicated appendicitis, Dr. Flum said. The CODA investigators studied patients who had an appendicolith together and separately from other patients.
The researchers randomly assigned 776 patients each to undergo appendectomy or receive a 10-day course of antibiotics administered intravenously for the first 24 hours and then as pills the remaining days.
Trade-offs with each treatment
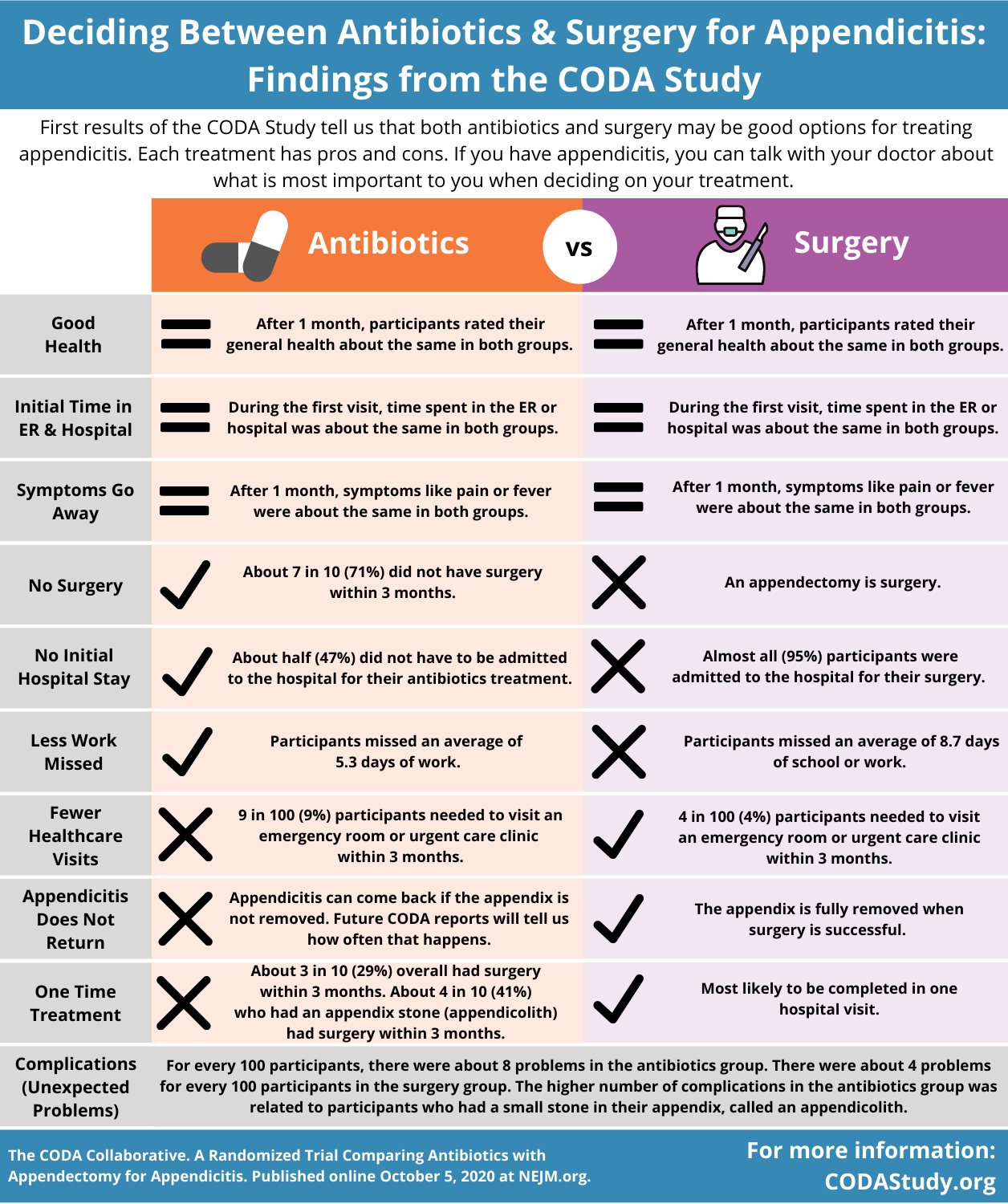
The main outcome was the patients’ health status 30 days after treatment using a measure of general health, the European Quality of Life-5 Dimensions (EQ-5D). Both treatment groups had similarly improved health on the EQ-5D, the investigators found, but each treatment had advantages and disadvantages.
Results for the antibiotics-alone group were as follows:
- The chance of needing an appendectomy by three months after the initial treatment was three in 10.
- The 90-day appendectomy rate was higher for patients with an appendicolith than those without: 41 percent versus 25 percent.
- Complications, although infrequent, appeared to be more common in those receiving antibiotics but was attributable to the appendicolith group.
- On average, patients missed 3.4 fewer days of work than those undergoing appendectomy (5.3 versus 8.7 days) but were likelier to need another hospitalization, including for an appendectomy (24 percent versus 5 percent).
- Forty-seven percent of patients received their initial care in the emergency department only and avoided hospitalization for initial treatment.
Without an appendectomy, there is a chance of missing a cancer of the appendix, but this type of cancer is rare, said Giana H. Davidson, MD, MPH, FACS, a study investigator and an associate professor of surgery at UW School of Medicine.
Patients with appendicitis need individualized treatment that meets their goals and needs, Dr. Davidson said.
Surgeons, she noted, may be concerned with a 30 percent appendectomy rate within three months of antibiotic treatment. This rate exceeded the 16 percent rate at 90 days reported privately by the lead investigator of the most recent and largest European trial, the Appendicitis Acuta (APPAC) trial.3 However, she said many study participants view the statistic differently.
“When you talk to some patients, depending on their personal priorities, health, and concerns, a 7 out of 10 chance that they won’t have to have an operation may be reasonable to them as long as it’s safe,” Dr. Davidson said.
A nonoperative treatment option may be especially relevant during the Coronavirus Disease 2019 (COVID-19) pandemic.
“When COVID hit, there were recommendations, including from the American College of Surgeons, to restrict time in the operating room to minimize exposure to the virus and reserve personal protective equipment for health care providers,” Dr. Davidson said. “We were getting calls from all over the country asking for our CODA data.”
Therefore, the researchers announced the 90-day findings ahead of the one- to three- year follow-up results expected in a year.
“This study is the largest randomized surgical trial of its kind in America. These initial results will be informative for surgeons and beneficial for patients as they discuss the most recent data-driven recommendations about treatment options for appendicitis,” said ACS Executive Director David B. Hoyt, MD, FACS, a member of the CODA National Advisory Board.
In addition to Dr. Flum, Dr. Talan, and Dr. Davidson, other article coauthors from the CODA Collaborative are: Sarah E. Monsell, MS, Nathan I. Shapiro, MD, MPH, Stephen R. Odom, MD, Sabrina E. Sanchez, MD, MPH, F. Thurston Drake, MD, MPH, Katherine Fischkoff, MD, Jeffrey Johnson, MD, Joe H. Patton, MD, Heather Evans, MD, Joseph Cuschieri, MD, Amber K. Sabbatini, MD, MPH, Brett A. Faine, PharmD, Dionne A. Skeete, MD, Mike K. Liang, MD, Vance Sohn, MD, Karen McGrane, MD, Matthew E. Kutcher, MD, Bruce Chung, MD, Damien W. Carter, MD, Patricia Ayoung-Chee, MD, MPH, William Chiang, MD, Amy Rushing, MD, Steven Steinberg, MD, Careen S. Foster, MD, Shaina M. Schaetzel, MD, Thea P. Price, MD, Katherine A. Mandell, MD, MPH, Lisa Ferrigno, MD, MPH, Matthew Salzberg, MD, Daniel A. DeUgarte, MD, Amy H. Kaji, MD, PhD, Gregory J. Moran, MD, Darin Saltzman, MD, PhD, Hasan B. Alam, MD, Pauline K. Park, MD, Lillian S. Kao, MD, Callie M. Thompson, MD, Wesley H. Self, MD, MPH, Julianna T. Yu, MD, Abigail Wiebusch, MD, Robert J. Winchell, MD, Sunday Clark, ScD, MPH, Anusha Krishnadasan, PhD, Erin Fannon, BA, Danielle C. Lavallee, PharmD, PhD, Bryan A. Comstock, MS, Bonnie Bizzell, MEd, Patrick J. Heagerty, PhD, and Larry G. Kessler, ScD.
For a listing of study sites click here.
The CODA Trial is funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (1409-24099).
Citation: A Randomized Trial Comparing Antibiotics and Appendectomy for Appendicitis (CODA). NEJM. DOI: 10.1056/NEJMoa2014320.
________________________
1 Flum DR, Davidson GH, Monsell SA, et al; CODA Collaborative. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. Posted online October 5, 2015. Available at: https://www.nejm.org/.
2 Newhall K, Albright B, Tosteson A, Ozanne E, Trus T, Goodney PP. Cost-effectiveness of prophylactic appendectomy: a Markov model. Surg Endosc. 2017 Sep;31(9):3596-3604.
3 Six clinical trials including the most recent: Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The APPAC randomized clinical trial. JAMA. 2015 Jun;313(23):2340-2348.
4 Sceats LA, Trickey AW, Morris AM, Kin C, Staudenmayer KL. Nonoperative management of uncomplicated appendicitis among privately insured patients. JAMA Surg. 2019 Feb;154(2):141-149.
# # #
About the American College of Surgeons
The American College of Surgeons is a scientific and educational organization of surgeons that was founded in 1913 to raise the standards of surgical practice and improve the quality of care for all surgical patients. The College is dedicated to the ethical and competent practice of surgery. Its achievements have significantly influenced the course of scientific surgery in America and have established it as an important advocate for all surgical patients. The College has more than 82,000 members and is the largest organization of surgeons in the world. For more information, visit www.facs.org.