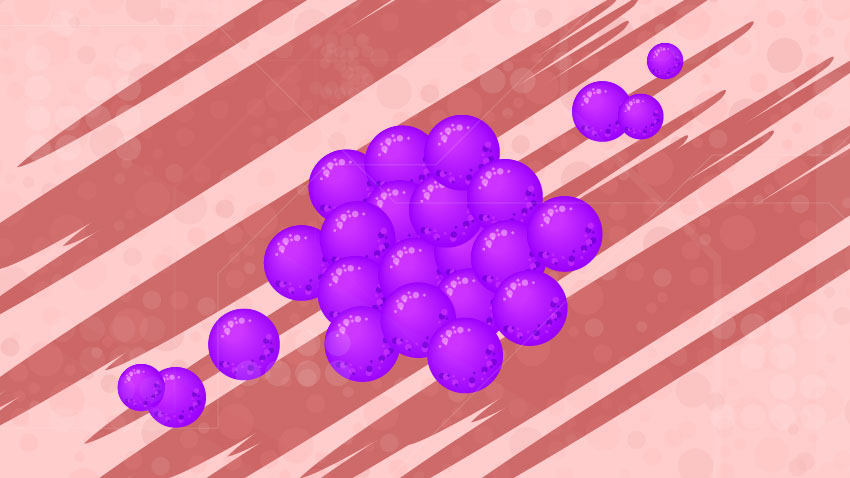
In the paper, published in the Journal of Investigative Dermatology, researchers found that 50% of skin rashes in patients with lupus contained an abnormally high presence of a common bacteria responsible for skin infections: staphylococcus aureus, or more commonly known as staph.
“Fifty percent of the patients we investigated were colonized by staph, which means the person with the rash is a carrier for the bacteria and can spread it to others,” says J. Michelle Kahlenberg, M.D., Ph.D., associate professor of rheumatology at Michigan Medicine and senior author of the paper.
“In addition, we identified that a protein in the skin of patients with lupus, called interferon, increases the stickiness of staph aureus to their skin.”
Kahlenberg had already done previous studies into interferons of the skin of patients with lupus.
“Because our previous work has shown the importance of interferons for sensitivity to sunlight and inflammation in lupus, we then wanted to study whether the interferons and staph were linked,” she says.
Kahlenberg notes that while skin rashes are a common side effect of lupus, she and her team were surprised by the abnormally high presence of staph colonization on the rashes.
“Using a University of Michigan lupus cohort, we found that patients with lupus had staph colonization on their skin at a rate higher than that reported in healthy adults – 40% compared to 30%,” Kahlenberg says. “And when the patients with lupus had active skin rashes or lesions, that rate increased to 50%.”
Kahlenberg says the focus on staph bacteria began because it’s a leading cause of infection in patients with lupus.
“Others have shown it may be associated with disease flares and development of lupus nephritis, or inflammation of the kidney in patients with lupus,” Kahlenberg says.
She is currently enrolling patients in a clinical trial that is testing whether topical antibiotics can decrease inflammation and rashes in the skin of patients with lupus.
“This is important because if true, the addition of topical antibiotics may be a simple way to improve treatment response in lupus skin and reduce the ability for those rashes to be colonized by staph,” Kahlenberg says.
For more information on the clinical trial, contact trial coordinator Rewaa Yas at [email protected].
Original post https://alertarticles.info