Vulnerable populations are more frequently treated at safety net hospitals because of the commitment to providing care regardless of ability to pay. These hospitals treat a higher proportion of Medicaid and uninsured patients, as well as a larger percentage of black and Hispanic patients and patients from poorer neighborhoods.
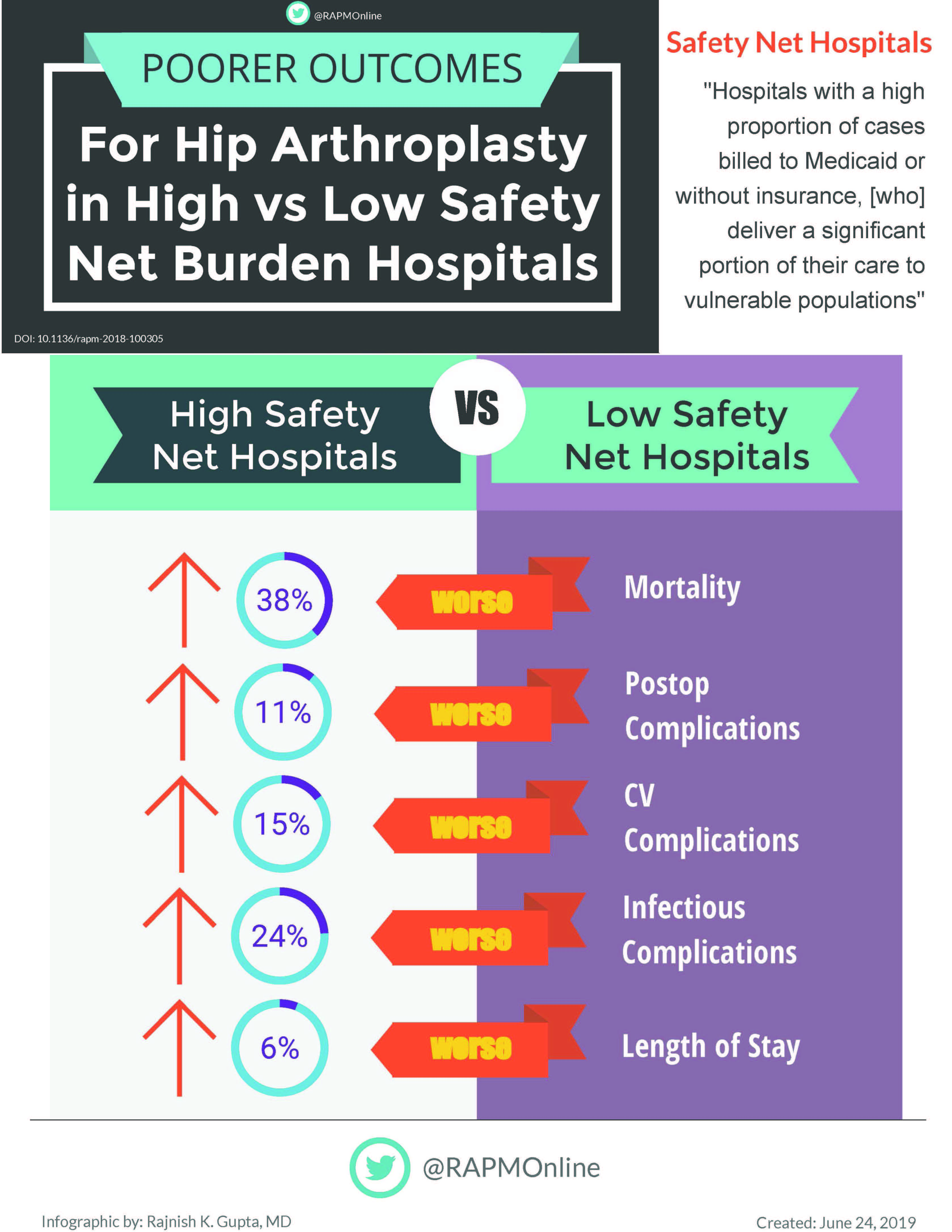
Patients who received hip replacement surgery at these kinds of hospitals – those that provide care regardless of ability to pay – were 38% more likely to die in the hospital than those receiving the surgery at other hospitals, according to a study published in Regional Anesthesia & Pain Medicine.
The study found that patient outcomes after receiving THA differed remarkably between hospitals categorized as “high burden” (i.e., those caring for a higher percentage of Medicaid/uninsured patients) and those defined as “low burden” (those treating more patients with private insurance). The patients treated at the high-burden hospitals were 11% more likely to develop postoperative complications and had 6% longer hospital stays than those treated at low-burden hospitals. In addition, cardiovascular complications were 15% higher and infection was 24% higher in patients at the high-burden facilities studied.
The researchers, who are from New York Presbyterian Hospital-Weill Cornell Medical College, looked at retrospective hospital discharge records from adults who underwent THA surgery from California, Florida, New York, Maryland, and Kentucky over a seven-year period. They were also able to look at whether patients in the New York state databases received general anesthesia (where the patient is unconscious) or regional anesthesia (which involves numbing specific areas of the body using local anesthesia). (This information was not available for the other states.) They found that high-burden safety net hospitals are 2.5 times more likely to use general anesthesia than regional anesthesia. Several studies have found that regional anesthesia is associated with fewer complications, less confusion, opioid consumption, blood loss, and even pain than general anesthesia. Therefore, its use may explain some of the improved outcomes at low burden hospitals.
The authors note that several studies have found associations between poor outcomes and high-burden safety net hospitals, but they state that this study may be the first comprehensive study on safety net burden and THA postoperative outcomes. High-burden safety net hospitals face financial disadvantages and resource limitations, among other challenges, which contributed to the disparities. They also note that anesthesiologists can have an influence on disparities. The use of evidence-based interventions, national guidelines, enhanced recovery pathways, and regional and multimodal anesthesia-analgesic regimens are some of the ways anesthesiologists can influence and reduce inequities. The American Society of Regional Anesthesia and Pain Medicine (ASRA) supports and promotes these and other objectives to improve patient outcomes.
Regional Anesthesia & Pain Medicine (www.rapm.org) is the official journal of ASRA. ASRA (www.asra.com) is a professional membership association of more than 5,000 physicians and healthcare providers, across 66 countries and 6 continues, committed to the advancement of the science and practice of regional anesthesia and pain medicine to improve patient outcomes through research, education, and advocacy. Our vision is to relieve the global burden of pain.
Original article here.
Hospital safety net burden is associated with increased inpatient mortality and postoperative morbidity after total hip arthroplasty: a retrospective multistate review, 2007–2014 Melvin La1, Virginia Tangel2, Soham Gupta2, Tiffany Tedore1, and Robert S White1
- Department of Anesthesiology, New York Presbyterian Hospital-Weill Cornell Medicine, New York City, New York, USA
- Center for Perioperative Outcomes, Department of Anesthesiology, Weill Cornell Medicine, New York City, New York, USA
Original post https://alertarticles.info