A new study by UT Southwestern shows artificial intelligence can identify a specific genetic mutation in a glioma tumor simply by examining 3D images of the brain – with more than 97 percent accuracy. Such technology could potentially eliminate the common practice of pretreatment surgeries in which glioma samples are taken and analyzed to choose an appropriate therapy.
Scientists across the country have been testing other imaging techniques in recent years, but the latest research describes perhaps one of the most accurate and clinically viable methods in the widespread effort to alter the paradigm of assessing brain cancer.
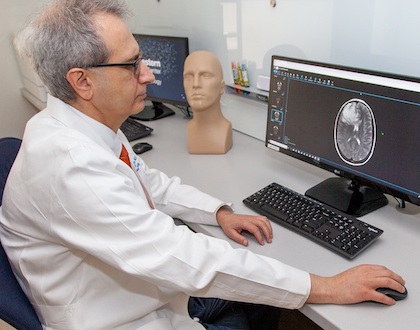
“Knowing a particular mutation status in gliomas is important in determining prognosis and treatment strategies,” says Joseph Maldjian, M.D., chief of neuroradiology at UT Southwestern’s O’Donnell Brain Institute. “The ability to determine this status using just conventional imaging and AI is a great leap forward.”
Mutated Enzymes
The study used a deep-learning network and standard magnetic resonance imaging (MRI) to detect the status of a gene called isocitrate dehydrogenase (IDH), which produces an enzyme that in mutated form may trigger tumor growth in the brain.
Doctors preparing to treat gliomas will often have patients undergo surgery to obtain tumor tissue that is then analyzed to determine the IDH mutation status. The prognosis and treatment strategy will vary based on whether a patient has an IDH-mutated glioma.
However, because obtaining an adequate sample can sometimes be time-consuming and risky – particularly if tumors are difficult to access – researchers have been studying non-surgical strategies to identify IDH mutation status.
The study, published this spring in Neuro-Oncology, differentiates itself from previous research in three ways:
- The method is highly accurate. Previous techniques have often failed to eclipse 90 percent accuracy.
- Mutation status was determined by analyzing only a single series of MR images, as opposed to multiple image types.
- A single algorithm was required to assess the IDH mutation status in the tumors. Other techniques have required either hand-drawn regions of interest or additional deep-learning models to first identify the boundaries of the tumor then detect potential mutations.
“The beauty of this new deep-learning model is its simplicity and high degree of accuracy,” says Maldjian, adding that similar methods may be used to identify other important molecular markers for various cancers. “We’ve removed additional pre-processing steps and created an ideal scenario for easily transitioning this into clinical care by using images that are routinely acquired.”
Tumor imaging
Gliomas comprise the strong majority of malignant tumors found in the brain and can often spread quickly through surrounding tissue. The five-year survival rate for high-grade gliomas is 15%, though tumors with mutated IDH enzymes generally have a better prognosis.
The IDH mutation status also helps doctors decide on a combination of treatments most suitable for the patient, from chemotherapy and radiation therapy to surgery to remove the tumor.
To improve the process of detecting enzyme mutations and deciding on appropriate therapy, Maldjian’s team developed two deep-learning networks that analyzed imaging data from a publicly available database of more than 200 brain cancer patients from across the U.S.
One network used only one series from the MRI (T2-weighted images), while the other used multiple image types from the MRI. The two networks achieved nearly the same accuracy, suggesting that the process of detecting IDH mutations could be significantly streamlined by using only the T2-weighted images.
‘Big picture’
Maldjian’s team will next test his deep-learning model on larger datasets for additional validation before deciding whether to incorporate the technique into clinical care.
Meanwhile, researchers are hoping to develop medications to inhibit IDH through ongoing national clinical trials. If effective, these inhibitors could combine with AI-imaging techniques to overhaul how some brain cancers are assessed and treated.
“In the big picture, we may be able to treat some gliomas without operating on a patient,” Maldjian says. “We would use AI to detect an IDH-mutated glioma, then use IDH inhibitors to slow down or reverse the tumor growth. The field of radio-genomics is exploding with possibilities.”
About the study
The study was supported with funds from the National Institutes of Health. Maldjian is a professor of radiology at UT Southwestern’s Peter O’Donnell Jr. Brain Institute and Advanced Imaging Research Center. He is the Lee R. and Charlene B. Raymond Distinguished Chair in Brain Research.
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty has received six Nobel Prizes, and includes 22 members of the National Academy of Sciences, 17 members of the National Academy of Medicine, and 14 Howard Hughes Medical Institute Investigators. The full-time faculty of more than 2,500 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in about 80 specialties to more than 105,000 hospitalized patients, nearly 370,000 emergency room cases, and oversee approximately 3 million outpatient visits a year.
Original post https://alertarticles.info