Millions around the world have waited for news about a COVID-19 vaccine, regarding it as the beginning of the end for the global pandemic and a herald for the eventual return to “normal life.”
Recent announcements from pharmaceutical companies Pfizer and Moderna that their respective late-stage vaccine trials have shown a 90% or better effectiveness rate have received international applause, excitement furthered with estimates that doses could be ready as early as December.
Unlike influenza (flu) inoculations, since these COVID-19 vaccines do not contain a dead or live sample of the virus, they are not produced using eggs but must be stored at frigid temperatures. Pfizer’s version requires a minus 70 degrees Celsius (-94°F) environment, which is more than four times as cold as the average kitchen freezer.
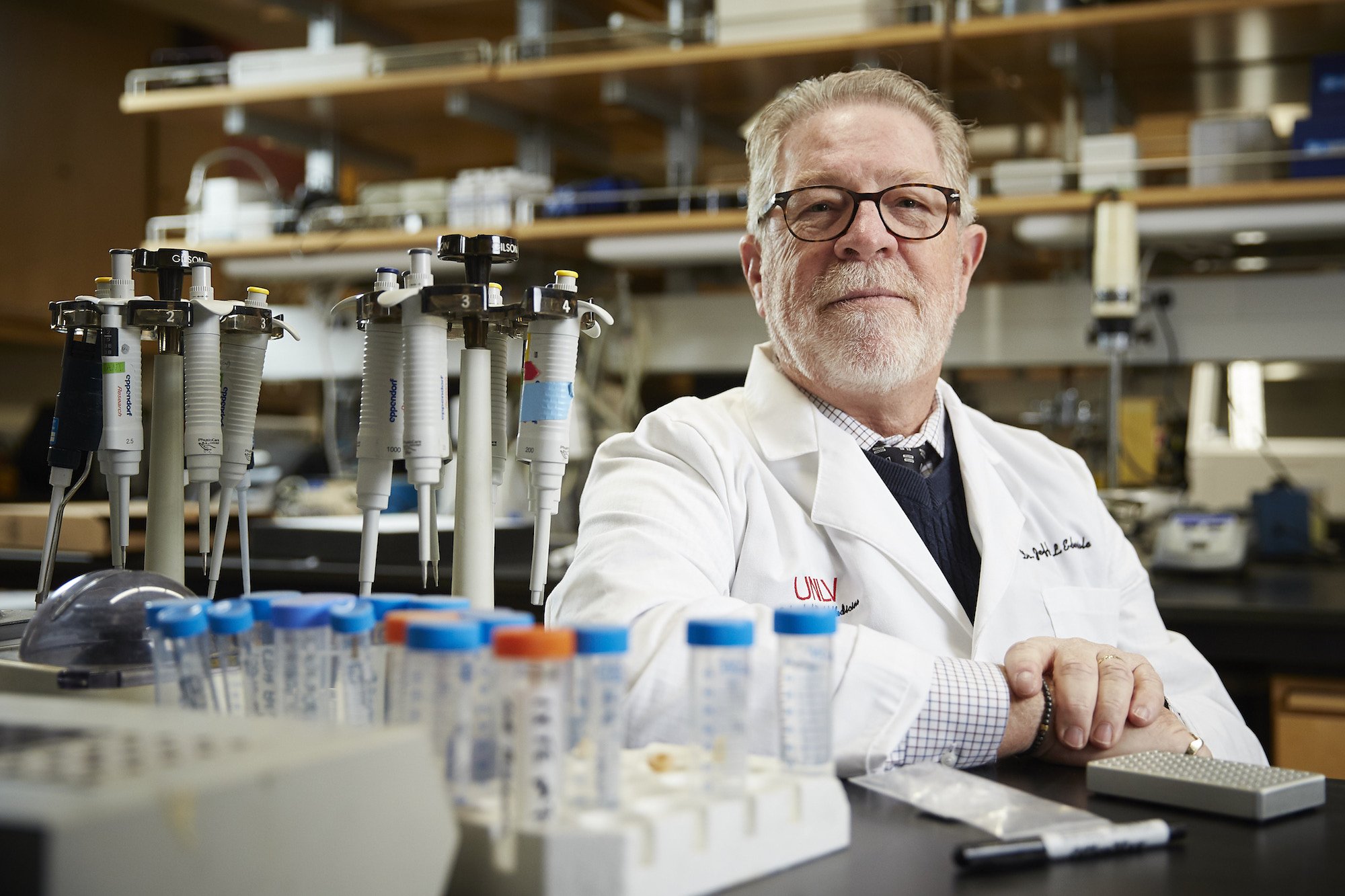
According to Dr. Jeffrey Ebersole, an immunologist and professor of biomedical sciences with UNLV’s School of Dental Medicine, both companies use nucleic acid technologies for their vaccines, which enables the vaccinated individuals’ immune systems to respond to a viral protein from the SARS-CoV-2 virus causing the infection.
“This process uses a very small part of the viral DNA that represents the critical spike protein, or the RNA that codes for this spike protein,” says Dr. Ebersole. “The RNA or DNA is ‘picked up’ by human cells – generally muscle cells at the site of injection – and stimulates the immune system’s protective response. These two vaccines are leading the “warp speed race” since both companies had been working prior to the pandemic on other viral vaccines using similar technology. They’re applying what had been learned from the SARS and MERS viruses of the previous decade, which infect in a similar fashion.
“However, because RNA and DNA in these vaccines are somewhat fragile, the low temperatures are necessary to keep the vaccines from breaking down and becoming ineffective,” he says.
Here, Dr. Ebersole explains in more detail how the leading vaccine candidates work and what makes them both different yet, hopefully, equally effective.
What’s the difference between RNA and DNA, and does use of one over the other make a particular vaccine better?
Basically, viral DNA is the fundamental instruction set that enables the creation of a live virus. The RNA is the transcript of the DNA that actually creates the proteins needed by the virus for life.
There is no evidence available from the existing data, nor theoretical scientific basis, that one should inherently be better than the other.
How are these vaccines different from others that may be developed?
While all vaccines are designed to induce antibodies that produce protection against infection and disease, one potential difference with the Pfizer and Moderna vaccines compared to other vaccines in development is that they may be less effective at inducing immune T cells. T cells circulate until they encounter their specific antigen – the part of the virus that triggers an immune response – rather than generically attacking any foreign particle.
This may be important since it’s still unclear why we’re seeing the extensive variation in disease presentation across the population, and exactly what aspects of the immune response are most effective in limiting infection/transmission and mitigating disease symptoms. Therefore, this T cell component could emerge to be an important aspect for broad and extended vaccine success.
Do we know if the vaccines will contain different strains of the virus, similar to a flu shot?
As this is a new type of coronavirus related to SARS and MERS, there is little evidence at this point that the identified COVID-19 strains are different enough to prevent the vaccines from working.
Just for clarification, a new flu vaccine is necessary yearly because the influenza virus and its genome have the ability to scramble the genetic code for two critical genes — hemagglutinin (H) and neuraminidase (N), which are crucial for its infectivity and pathogenicity. This is where we get the designation of strains like H1N1. Each year a new mix of the H and N genes translocate across the globe. That’s why public health, infectious disease, and epidemiology specialists work to predict as early as possible what the likely combination will be for any given year.
Most often, the specialists are pretty much on point. Sometimes the guesstimate is not as good and we witness higher global infection rates and need a new specific flu vaccine to be produced as the flu season progresses. Currently, it does not appear that the coronavirus family of viruses expresses this type of major and rapid change.
According to the news, one of the two vaccines has a slightly higher rate of efficacy. Could both be approved and distributed for use?
The differences in effectiveness reported between the Pfizer and Moderna vaccines are not substantial regarding approval and distribution. While each of the Phase 3 trials have included vaccinating 15,000 to 20,000 people (1/2 of the study population), translating effectiveness differences among 100 million to 300 million people, who represent extreme heterogeneity reflecting genetic and environmental differences, really can’t be discerned at this point in the process.
Both appear safe within the limitations of the population tested and timeline of follow-up, and both appear to be similarly effective.