Researchers in China have discovered how brain cancer cells increase production of a key protein that allows them to evade the body’s immune system. The study, which will be published August 27 in the Journal of Experimental Medicine (JEM), suggests that targeting this cellular pathway could help treat the deadly brain cancer glioblastoma, as well as other cancers that are resistant to current forms of immunotherapy.
Immune cells known as cytotoxic T cells can prevent tumor growth by attacking and killing cancer cells. To avoid this fate, many cancer cells produce a protein called PD-L1 that deactivates T cells by binding to a protein called PD-1 on the surface of the immune cells. Immunotherapies that block the interaction between PD-L1 and PD-1 can reactivate cytotoxic T cells and cause tumor regression in melanoma and non–small cell lung cancer patients, and clinical trials are currently assessing this approach for several other types of cancer, including the aggressive brain cancer glioblastoma.
“However, the underlying mechanisms of PD-L1 regulation in glioblastoma remain unclear,” says Jianxin Lyu, a professor at Wenzhou Medical University in China and co–senior author of the paper.
In the new study, Lyu and colleagues, including co–senior author Zhimin Lu from Zhejiang University School of Medicine, identified two cell-signaling pathways that drive the production of PD-L1 in glioblastoma cells. These two pathways, known as Wnt signaling and EGF signaling, stabilize a protein called β-catenin, allowing it to enter the cell nucleus and activate the gene encoding PD-L1.
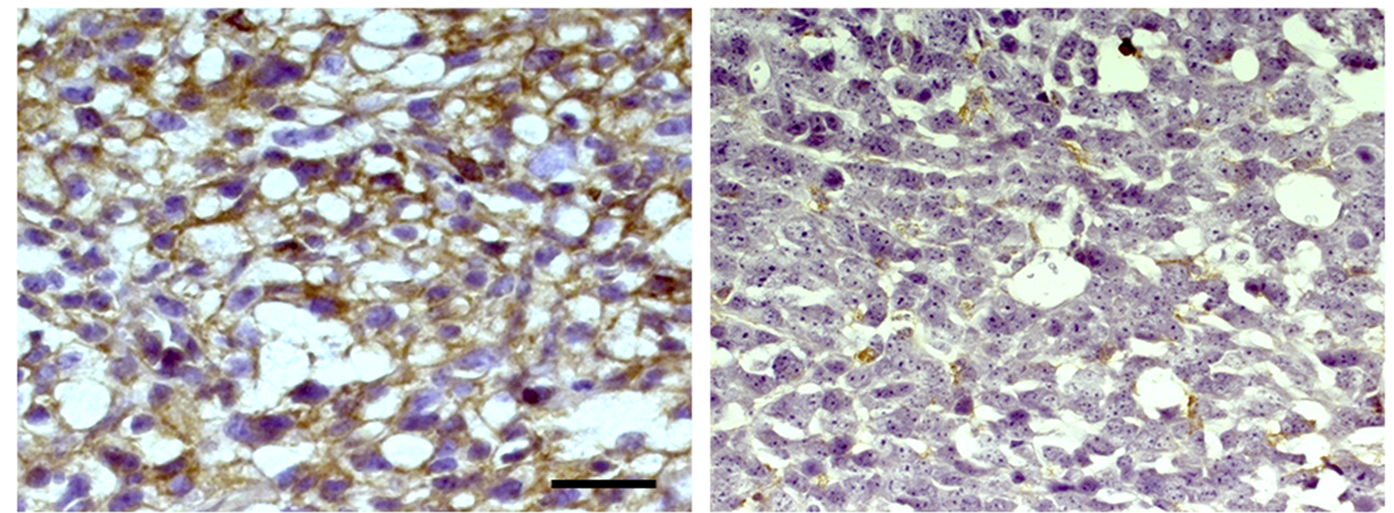
Lyu and colleagues found that treating mice with a drug, MK2206, that inhibits this pathway reduced the production of PD-L1 by glioblastoma cells and increased the number of active T cells targeting their brain tumors. This, in turn, reduced tumor growth and prolonged the animals’ survival. “Combining MK2206 with an anti–PD-1 antibody further enhanced T cell infiltration and was even more effective at blocking tumor growth,” Lyu says.
The researchers found that glioblastoma patients with mutations activating this signaling pathway show increased levels of PD-L1 and reduced numbers of T cells within their brain tumors. “Our data demonstrates that EGF and Wnt signaling, which is often active in a wide variety of cancers, induce the upregulation of PD-L1,” says Lyu. “Our results therefore provide a molecular basis for improving the clinical response rate and efficacy of anti–PD-1/PD-L1 immunotherapy in cancer patients.”
Du et al., 2020. J. Exp. Med. https://rupress.org/jem/article-lookup/doi/10.1084/jem.20191115?PR
# # #
About the Journal of Experimental Medicine
The Journal of Experimental Medicine (JEM) features peer-reviewed research on immunology, cancer biology, stem cell biology, microbial pathogenesis, vascular biology, and neurobiology. All editorial decisions are made by research-active scientists in conjunction with in-house scientific editors. JEM makes all of its content free online no later than six months after publication. Established in 1896, JEM is published by Rockefeller University Press. For more information, visit jem.org.
Visit our Newsroom, and sign up for a weekly preview of articles to be published. Embargoed media alerts are for journalists only.
Follow JEM on Twitter at @JExpMed and @RockUPress.