In experiments in rats and mice, two Johns Hopkins scientists — an engineer and an ophthalmologist — report the successful use of nanoparticles to deliver gene therapy for blinding eye disease. A uniquely engineered large molecule allows researchers to compact large bundles of therapeutic DNA to be delivered into the cells of the eye.
The research, described July 3 in Science Advances, provides evidence of the potential value of nanoparticle-delivered gene therapy to treat wet age-related macular degeneration — an eye disease characterized by abnormal blood vessel growth that damages the light-sensitive tissue in the back of the eye — as well as more rare, inherited blinding diseases of the retina.
Many gene therapy approaches depend on viral vectors, which use a virus’s natural ability to carry genetic material into cells. However, viruses create an immune response, which prevents repeat dosing, and the most commonly used one for ocular gene therapy cannot carry large genes.
“Some of the most prevalent inherited retinal degenerations are due to mutations in large genes that simply cannot fit into the most commonly used viral vector,” says Peter Campochiaro, M.D., the Eccles Professor of Ophthalmology at the Johns Hopkins University School of Medicine, and a member of the Johns Hopkins Medicine Wilmer Eye Institute.
To overcome such limitations, Campochiaro and Jordan Green, Ph.D., developed a new approach involving a biodegradable polymer that surrounds and compacts long stretches of DNA, creating nanoparticles that can enter the cells. This technology allows the researchers to convert the cells of the eye into minifactories for a therapeutic protein.
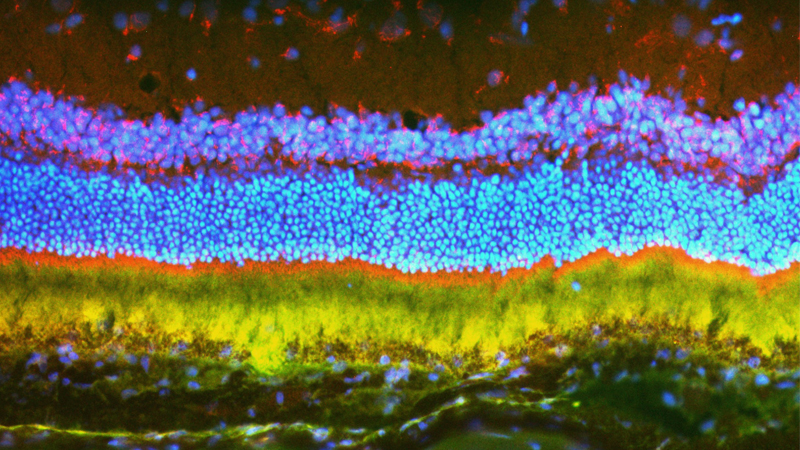
To first test whether the nanoparticles could reach their target cells, the researchers loaded the nanoparticles with a gene for a florescent protein that causes cells to light up like a glow stick.
This glowing molecule allowed the researchers to determine the location, amount and duration of gene expression achievable with the nanoparticles.
They found that even eight months after treatment, the majority of the light-sensitive cells in the rats’ eyes glowed, showing that the nanoparticles effectively deposited the florescent gene into the cells.
Next, the researchers set up a similar experiment, this time using the nanoparticles to shuttle a biologically relevant gene into the eye. They loaded the nanoparticles with a gene for vascular endothelial growth factor (VEGF), which is responsible for the growth of abnormal blood vessels in people with wet macular degeneration.
The researchers injected the eyes of 30 rats with the nanoparticles carrying the VEGF gene and determined the effects in the retina one, two and five months after injection. One month after injection, each rat tested had developed abnormal blood vessels under and within the retina, like those seen in patients with wet macular degeneration. The abnormal blood vessels were more extensive at two and five months after injection, and there was associated scarring under the retina similar to that seen in chronic untreated wet macular degeneration.
“These results show that the genes delivered by nanoparticles stayed active within the cells for several months,” says Campochiaro.
Finally, to test a nanoparticle’s ability to deliver a therapeutic gene for the disease, the researchers used mice genetically engineered to develop a form of wet macular degeneration similar to that in humans. The researchers loaded nanoparticles with a gene that produces a protein that neutralizes VEGF.
Currently, physicians inject such proteins that block VEGF proteins into the eyes of people with macular degeneration, a treatment that helps control the overgrowth of abnormal, leaky blood vessels. But this procedure must be repeated frequently and is burdensome for patients and their caretakers.
Three weeks after injecting nanoparticles containing the gene for the anti-VEGF protein, the mice had a 60% reduction in abnormal blood vessels when compared to control mice. The same effect was seen 35 days later.
“These results are extremely promising,” says Jordan Green, Ph.D., professor of biomedical engineering at the Johns Hopkins University School of Medicine. “We have the ability to reach the cells most significantly affected by degenerative eye disease with nonviral treatments that can allow the eye to create its own sustained therapies.”
An estimated 1.6 million people in the U.S. with macular degeneration receive injected drugs to the eye every four to six weeks. A gene therapy treatment could provide a way for the eye’s tissue to prevent further vision deterioration with as little as a few initial treatments. Genetic diseases that cause blindness could be treated in a similar way, by introducing functional versions of genes that inherited mutations have disabled.
Other researchers involved in this study include Jikui Shen, Jayoung Kim, Stephany Tzeng, Kun Ding, Zibran Hafiz, Da Long and Jiangxia Wang of the Johns Hopkins University School of Medicine.
This research was supported by the National Eye Institute (01EY031097, R21EY026148, R01EY028996, EY01765), the National Institute of Biomedical Imaging and Bioengineering (R01EB022148) Research to Prevent Blindness (the Dr. H. James and Carole Free Catalyst Award and an unrestricted grant), the Louis B. Thalheimer Fund for Translational Research; the Barth Syndrome Foundation, Samsung, Conrad and Lois Aschenbach, Per Bang-Jensen, Andrew and Yvette Marriott, and Jean Lake.
No authors declared conflicts of interest related to this research under Johns Hopkins University School of Medicine policies.
Original post https://alertarticles.info