CHICAGO: Surgical patients who participate in virtual follow-up visits after their operations spend a similar amount of time with surgical team members as those who meet face-to-face. Moreover, these patients benefit by spending less time waiting at and traveling to the clinic for in-person appointments, according to research findings presented at the virtual American College of Surgeons Clinical Congress 2020.
“I think it’s really valuable for patients to understand that, in the virtual space scenario, they are still going to get quality time with their surgical team,” said lead study author Caroline Reinke, MD, FACS, associate professor of surgery at Atrium Health in Charlotte, N.C. “A virtual appointment does not shorten that time, and there is still an ability to answer questions, connect, and address ongoing medical care.”
Due to the Coronavirus Disease 2019 (COVID-19) pandemic and the widespread adoption of technology, many surgical patients are being offered virtual appointments in place of traditional in-person visits. The researchers say this is one of the first studies to look at how patients spend their time in post-operative virtual visits compared with face-to-face consultations.
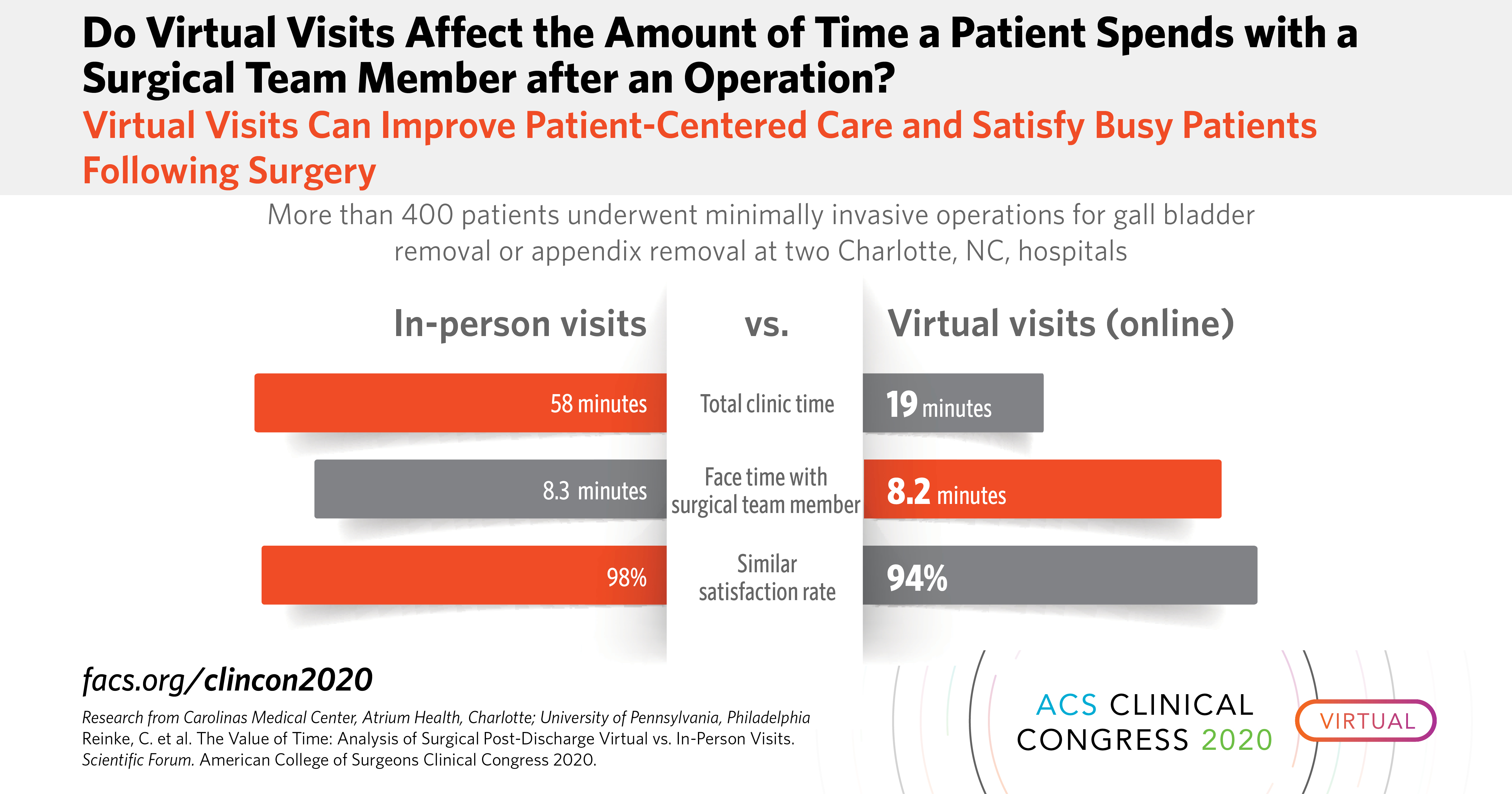
The study design was a non-inferiority, randomized controlled trial that involved more than 400 patients who underwent laparoscopic appendectomy or cholecystectomy at two hospitals in Charlotte, N.C. and were randomized 2:1 to a post-discharge virtual visit or to an in-person visit. The study began in August 2017 but was put on hold in March 2020 due to COVID-19.
“Other studies have looked at the total visit time, but they haven’t been able to break down the specific amount of time the patient spends with the provider. And we wanted to know if that was the same or different between a virtual visit and an in-person visit,” Dr. Reinke said. “We wanted to get down to the nitty gritty of how much face time was actually being spent between the surgical team member and the patient.”
Researchers tracked total time the patients spent checking in, waiting in the waiting room and exam room, meeting with the surgical team member, and being discharged after the exam. For in-person visits, on-site waiting time and an estimated drive time was factored into the overall time commitment.
Just 64 percent of patients completed the follow-up visit. “Sometimes, patients are doing so well after minimally invasive surgery that about 30 percent of these patients don’t show up for a post-operative visit,” Dr. Reinke said.
Overall, results showed that the total clinic time was longer for in-person visits than virtual visits (58 minutes vs. 19 minutes). However, patients in both groups spent the same amount of face time with a member of their surgical team (8.3 minutes vs. 8.2 minutes) discussing their post-operative recovery.
“I was pleasantly surprised that the amount of time patients spent with the surgical team member was the same, because one of the main concerns with virtual visits is that patients feel disconnected and that there isn’t as much value in it,” Dr. Reinke said.
Importantly, patients placed a high value on convenience and flexibility. “We received overwhelmingly positive responses to this patient-centered care option.” Dr. Reinke said. “Patients were able to do the post-operative visit at work or at home while caring for children, without having to disrupt their day in such a significant way.”
The researchers also found that patients embraced the virtual scenario. The satisfaction rate between both groups of patients was similar (94 percent vs. 98 percent).
In addition, wait time was much less for patients who got virtual care. “Even for virtual visits, the amount of time the patients spent checking in and waiting was about 55 percent of total time. Because virtual visits have the same regulations as in-person visits, even if you take out the components of waiting room and patient flow within the clinic, patients are still spending about half of their time on the logistics of check in,” Dr. Reinke. “Yet, with virtual visits, there is still much less time spent waiting, about 80 percent less time.”
Still, some patients are not comfortable with the technology. The number of patients who couldn’t or didn’t want to do a virtual visit was higher than expected, according to the authors.
“I think there are some patients that would really just rather come in and shake someone’s hand,” Dr. Reinke said. “I think for surgery it’s a little bit different, because with surgical care there are incisions to check on. However, we were able to check on incisions pretty easily, having patients show us their incisions virtually on the video screen.”
Coauthors are Kristen Harkey, DNP; Nicole Kaiser, BS; Brent Duane Matthews, MD, FACS; Rachel Kelz, MD, FACS; and Michael Inman, BS.
This research was supported by the American College of Surgeons Franklin H. Martin Faculty Research Fellowship.
“FACS” designates that a surgeon is a Fellow of the American College of Surgeons.
Citation: The Value of Time: Analysis of Surgical Post-Discharge Virtual vs. In-Person Visits. Scientific Forum, American College of Surgeons Clinical Congress 2020, October 3-7, 2020.
# # #
About the American College of Surgeons The American College of Surgeons is a scientific and educational organization of surgeons that was founded in 1913 to raise the standards of surgical practice and improve the quality of care for all surgical patients. The College is dedicated to the ethical and competent practice of surgery. Its achievements have significantly influenced the course of scientific surgery in America and have established it as an important advocate for all surgical patients. The College has more than 82,000 members and is the largest organization of surgeons in the world. For more information, visit www.facs.org.