While most adults over 50 understand that overuse of antibiotics is a problem, and say they’re cautious about taking the drugs, a sizable minority have used antibiotics for something other than their original purpose, and appear to think the drugs could help treat colds, which are caused by viruses not bacteria.
These findings, contained in a new paper in Infection Control and Hospital Epidemiology, come from a national poll of people between the ages of 50 and 80 carried out as part of the National Poll on Healthy Aging.
The authors, from the University of Michigan’s Institute for Healthcare Policy and Innovation, say their findings highlight the importance of careful guidance from health care providers to older adults, about the proper use and disposal of antibiotics prescribed to outpatients.
The paper expands on the findings first shared in an NPHA report in late 2019. The national poll included responses from more than 2,200 adults who were asked if they had received a prescription for an antibiotic at least once in the last two years, and also about their past practices before the two-year window.
Key data from the new paper:
- More than 91% of older adults said they are cautious about using antibiotics, and nearly 89% agreed that overuse can lead to antibiotics not working the next time they’re needed.
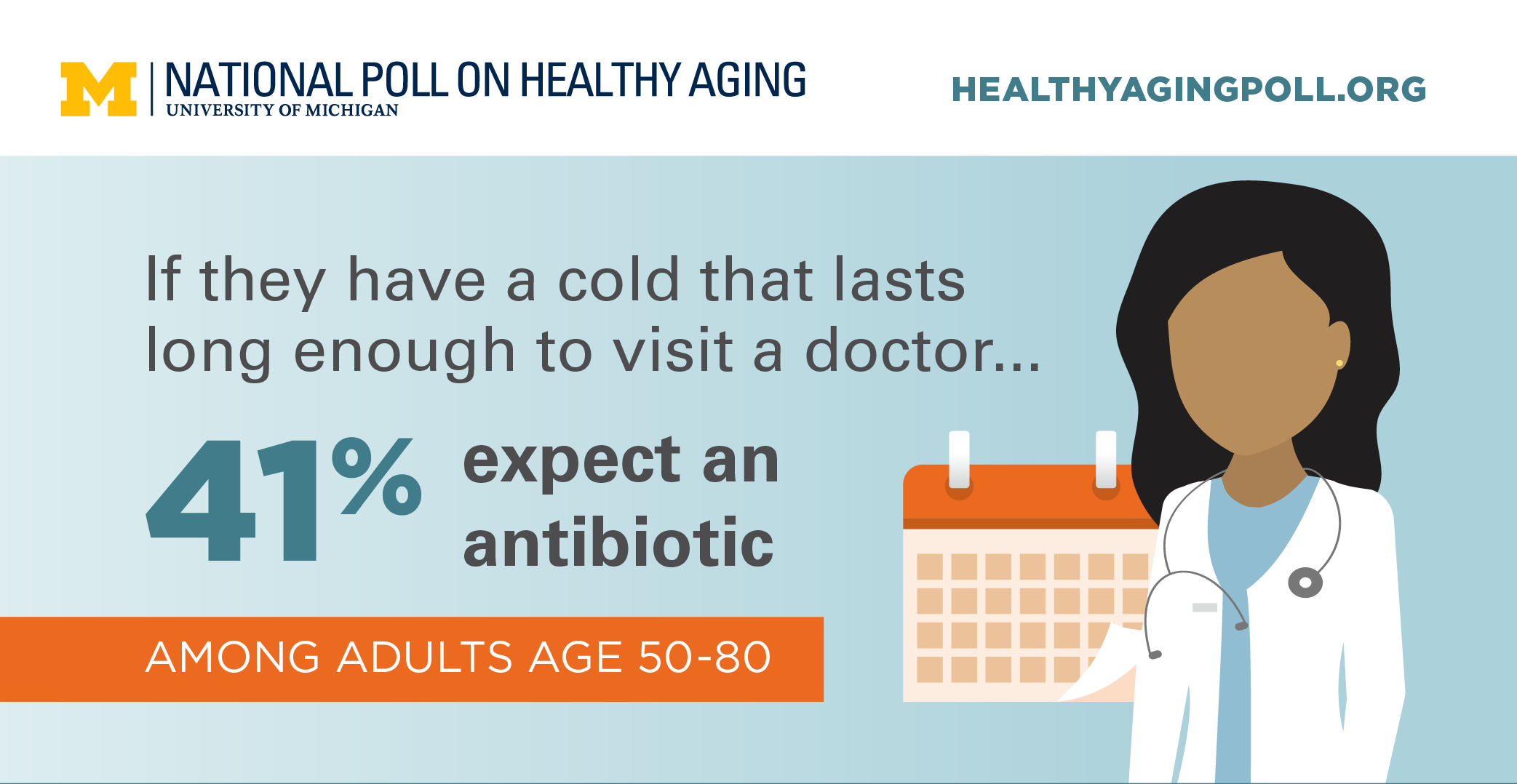
- Nearly 56% agreed that doctors overprescribe antibiotics, but 41% said that if they had a cold or flu that lasted long enough to cause them to see a doctor, they would expect to receive a prescription for an antibiotic.
- 34% said they believe antibiotics can help them get better if they get a cold or the flu; these conditions are viral illnesses that do not respond to antibiotics, which aim to kill infectious bacteria.
- Nearly 48% of older adults had received at least one prescription for antibiotics in the past two years, and half of these said at least one prescription was for a respiratory condition.
- Nearly 13% of those who filled an antibiotic prescription said they had leftover medication, even though antibiotics are typically prescribed as “courses” that are intended to be taken until no medication remains. Stopping a prescription early can increase the chance that the surviving bacteria will evolve resistance to future treatment by antibiotics.
- 65% of those with leftover antibiotics said they kept them, and nearly 60% of these respondents said they did so in case they needed the medication in the future. This practice is not recommended; experts say individuals should seek medical attention for new signs of infection, and obtain a new prescription if antibiotics are warranted.
- Nearly 19% of all respondents said that they had taken antibiotics without talking to a health care professional at least once in the past, and most said they had taken their own leftover antibiotics.
- Among those who said they had had leftover antibiotics from a prescription in the past two years, just over 50% said they had taken the leftovers without talking to a healthcare professional.
The poll, based at IHPI, is supported by AARP and Michigan Medicine, the University of Michigan’s academic medical center. The study’s authors are NPHA director Preeti Malani, M.D. and associate directors Jeffrey Kullgren, M.D., M.S., M.P.H., and Erica Solway, Ph.D., M.S.W., M.P.H., as well as poll team members Matthias Kirch, M.S. and Dianne Singer, M.P.H.
Reference: Use and perceptions of antibiotics among US adults aged 50–80 years, Infection Control & Hospital Epidemiology, DOI: https://doi.org/10.1017/ice.2021.19