LOS ANGELES (Oct. 3, 2024) — Patients who take a class of widely prescribed medications to manage diabetes and obesity may require extra preparations before undergoing upper endoscopy procedures, according to a new Cedars-Sinai study.
The drugs, known as glucagon-like peptide-1 receptor agonists (GLP-1RAs), are marketed under many brand names. They work by stimulating insulin secretion, slowing down food leaving the stomach, and causing a delay in gastric emptying. As a result, the drugs may help Type 2 diabetes patients manage their blood sugar and help patients with obesity to lose weight.
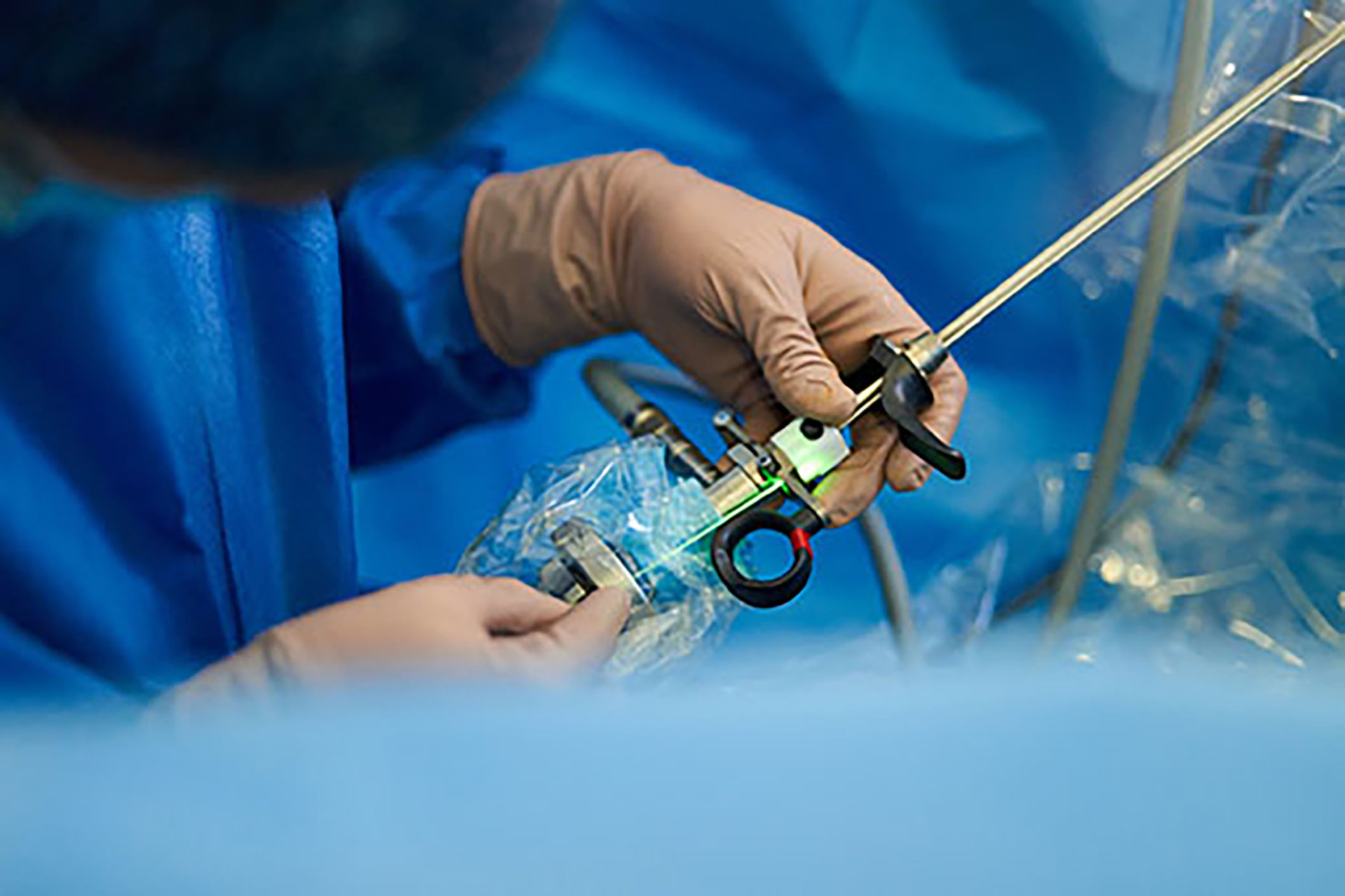
According to the study, published Oct. 1 in the journal JAMA Network Open, these medications may also lead to problems during upper endoscopies, which involve inserting an endoscope—a long, thin tube with a camera and a light on the end—into a patient’s esophagus, stomach and the beginning of the small intestine under sedation to diagnose diseases and conditions of the digestive system.
Researchers found that patients who regularly took GLP-1RAs were significantly more likely to retain food in their stomachs during the procedure than were patients who did not take the drugs. Food retention can raise the risk of aspiration, a rare but serious complication of surgeries in which stomach contents are introduced into the lungs while a patient is under sedation.
The researchers found that even though patients in the study, as instructed, stopped taking the GLP-1RAs a week before their upper endoscopies, they were still more likely to retain food than those who did not take these drugs.
“The effects of the GLP-1RA drugs appeared to persist even when patients were asked to stop taking them a week before the procedure,” said endocrinologist Ruchi Mathur, MD, professor of Medicine, director of Clinical Research and Clinical Operations for Medically Associated Science and Technology at Cedars-Sinai and the study’s corresponding author. She added that although aspiration was not detected in any of the patients, food retention can make aspiration more likely.
A total of 70 individuals taking GLP-1RAs and 139 controls were included in the study.
Results showed that 17% of patients on the drugs who underwent upper endoscopy alone showed food retention, compared with none of the controls. They also observed that patients who underwent both a colonoscopy and an upper endoscopy on the same day, requiring a 24-hour clear liquid and bowel preparation protocol, showed no food retention in either the GLP-1RA group or the controls. “This protective effect against food retention may be due to the preparation typically required for colonoscopies, as opposed to upper endoscopies,” Mathur said.
The researchers also found a clear association between GLP-1RA use, which can sometimes produce constipation as a side effect, and unsatisfactory bowel preparation for colonoscopies. Inadequate bowel preparation may contribute to missed lesions, patient dissatisfaction, and cancellation of the procedure.
“Overall, our results support the value of individualizing recommendations for patients and having risk-benefit discussions for patients on these drugs,” Mathur said. “Any patients using a GLP-1RA drug should be sure to inform their physicians and anesthesiologists before undergoing gastrointestinal procedures.”
Peter Chen, MD, professor of Medicine, the Medallion Chair in Molecular Medicine and interim chair of the Cedars-Sinai Department of Medicine, said, “The rigorous research performed by Dr. Mathur and her team represents an important contribution to our understanding of how these powerful obesity and diabetes medications may impact medical care.”
Other Cedars-Sinai authors include Jason Nasser, MD; Ava Hosseini, MPH; Gillian Barlow, PhD; Roma Gianchandani, MD; Ali Rezaie, MD, MSc; and Mark Pimentel, MD.
Follow Cedars-Sinai Academic Medicine on LinkedIn for more on the latest basic science and clinical research from Cedars-Sinai.