Unlike many other cancers, most pancreatic tumors are rock hard.
“That’s one reason why pancreatic cancer is one of the most lethal types of cancer,” says Kenneth Olive, PhD, associate professor of medicine and pathology & cell biology at Columbia University Vagelos College of Physicians and Surgeons and a pancreatic cancer researcher at the Herbert Irving Comprehensive Cancer Center.
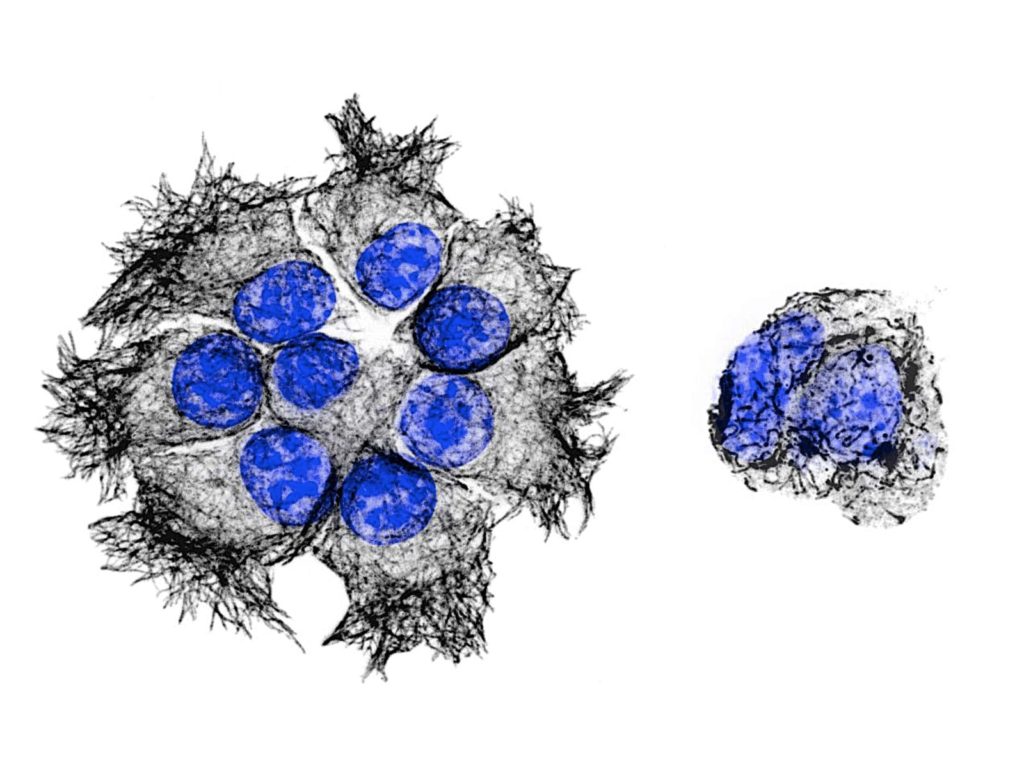
“Pancreatic tumors recruit a thick layer of connective tissue called stroma that hardens the tumor and acts like a shield,” says Olive, whose previous research first uncovered how the stroma makes it difficult for chemotherapy drugs to reach malignant cells. “As a result, most chemotherapy drugs can’t build up to the levels needed to be effective.”
To Olive, that suggests, paradoxically, a longer-lived—but less toxic—drug may work better.
“For a pancreatic cancer drug to be effective, it needs to stick around long enough to seep past the stroma and accumulate in the tumor. But if it is going to persist for a long time in the blood, it can’t be as toxic to the rest of the body,” he says.
Testing a New Drug Combination
Olive’s latest research, which was led by Jaime Eberle-Singh, PhD, while she was a graduate student at Columbia, may have identified a good candidate. The drug, an experimental compound called PTC596 that had shown antitumor activity in mouse and human pancreatic cancer cells, seemed to have the right qualities: PTC596 has a durable half-life (most cancer drugs have a half-life of a few minutes to hours) and can evade a pump that many cancer cells use to expel drugs. “This means that any amount of drug that makes it past the barrier can target the malignant cells,” says Olive.
Based on those studies, Olive, Eberle-Singh, and their collaborators tested PTC596 in combination with gemcitabine (a first-line drug for pancreatic cancer) in genetically engineered mice with an aggressive form of pancreatic cancer that is generally resistant to chemotherapy.
The mice that were treated with the two-drug combination lived three times longer than those treated with only a single standard agent. “This result was exciting because it’s exceedingly rare for any treatment to extend survival in this gold-standard mouse model,” Olive says.
They also tested PTC596 in combination with gemcitabine and another drug commonly used to treat pancreatic cancer, nab-paclitaxel, using human pancreatic tumors grown in mice. This combination further enhanced efficacy, making the tumors shrink outright.
“Based on the drug’s safety profile and our own findings, there’s a good rationale for testing PTC596 in combination with standard therapy in patients with pancreatic cancer,” says Olive.
Microtubule Breakdown
Olive’s team also discovered that PTC596 blocks the formation of microtubules—a network of proteins involved in cell division and transport of nutrients within the cell. He demonstrated that PTC596 may act synergistically with nab-paclitaxel, another microtubule-binding agent.
“Combining different microtubule inhibitors has the potential to play an important role in the future of oncology, as there are many agents that each impact microtubules in different ways that could produce synergy,” Olive says.
Additional Information
The article is titled “Effective delivery of a microtubule polymerization inhibitor synergizes with standard regimens in models of pancreatic ductal adenocarcinoma” and was published in Clinical Cancer Research.
Additional authors are Jaime A. Eberle-Singh (Columbia University Irving Medical Center, New York, NY), Irina Sagalovskiy (CUIMC), H. Carlo Maurer (CUIMC), Stephen A. Sastra (CUIMC), Carmine F. Palermo (CUIMC), Amanda R. Decker (CUIMC), Min Jung Kim (PTC Therapeutics, South Plainfield, NJ), Josephine Sheedy (PTC Therapeutics), Anna Mollin (PTC Therapeutics), Liangxian Cao (PTC Therapeutics), Jianhua Hu (CUIMC), Arthur Branstrom (PTC Therapeutics), and Marla Weetall (PTC Therapeutics).
The research was supported by the National Cancer Institute (1R21CA188857), the Stewart Trust Cancer Research Fellowship, and sponsored research support from PTC Therapeutics.
Min Jung Kim, Josephine Sheedy, Anna Mollin, Liangxian Cao, Arthur Branstrom, and Marla Weetall are employees of PTC Therapeutics, which discovered and is developing PTC596. The laboratory of Kenneth Olive received partial funding for this work through a sponsored research agreement between Columbia University and PTC Therapeutics. No personal compensation or incentive was provided. Dr. Olive is a member of the scientific advisory board of Elstar Therapeutics; there is no relationship between Elstar and the work presented in this manuscript.
###
Columbia University Irving Medical Center provides international leadership in basic, preclinical, and clinical research; medical and health sciences education; and patient care. The medical center trains future leaders and includes the dedicated work of many physicians, scientists, public health professionals, dentists, and nurses at the Vagelos College of Physicians and Surgeons, the Mailman School of Public Health, the College of Dental Medicine, the School of Nursing, the biomedical departments of the Graduate School of Arts and Sciences, and allied research centers and institutions. Columbia University Irving Medical Center is home to the largest medical research enterprise in New York City and State and one of the largest faculty medical practices in the Northeast. For more information, visit cuimc.columbia.edu or columbiadoctors.org.