DALLAS – March 8, 2021 – A new type of CAR T-cell therapy more than triples the expected length of remission for multiple myeloma patients who have relapsed several times, according to an international clinical trial with UT Southwestern as the lead enrolling site.
Results of the trial, published recently in the New England Journal of Medicine, were significantly better than those seen with other therapies available to heavily relapsed and refractory myeloma patients who had already received the three main classes of treatment. Nearly three-quarters of the patients had at least a partial response to the therapy. About a third achieved a complete remission, with the disappearance of all traces of cancer.
Median time without the disease worsening was 8.8 months with this new treatment, but Larry D. Anderson Jr., M.D., Ph.D., associate professor of internal medicine and co-first author of the journal article, points out that patients who received the trial’s maximum dose of engineered T-cells experienced longer remissions, bringing the average to more than 12 months. Previously, similar patients treated with currently available therapies following multiple relapses have only had an average of three to four months of remission before their disease returned.
“We have patients that are over two years out from their single infusion of CAR T-cells and still in remission despite having no other treatment options when they were enrolled in this trial,” says Anderson, a member of the Harold C. Simmons Comprehensive Cancer Center who cares exclusively for patients with plasma cell disorders, mostly myeloma patients. “The results mark a true breakthrough with unprecedented depth and duration of remissions from what we hope will be the first cellular therapy option to become available for myeloma patients. Even though we don’t yet know if some of these patients may be cured, and many relapse within one to two years, it can at least buy many patients time until other treatment options become available. Most patients also have good quality of life with relatively low risk of severe CAR T-cell-related side effects.”
Multiple myeloma, the second most common blood cancer, is a cancer of plasma cells, a white blood cell important in the immune system. The disease’s attack on bone marrow puts patients at risk of life-threatening infections. It is diagnosed in more than 32,000 people a year, and African Americans are twice as likely as the general population to be diagnosed with this disease.
Three main classes of treatment are available now for multiple myeloma: drugs called proteasome inhibitors, drugs to modulate the immune system, and antibody treatments. Among more than a dozen new therapies for myeloma approved by the Food and Drug Administration over the past decade, most offer only a few months of remission for patients with multiple relapses. Until now, most treatments induce responses in only a third of patients, and complete remissions are rare.
The phase 2 trial involved 128 patients, ages 18 and older, who previously had been given regimens from the three main classes of treatment. The patients received a median of six previous antimyeloma regimens; 120 formerly had undergone stem cell transplantation.
The clinical trial included nine sites in the U.S., one in Canada, and 10 sites in five European countries. Several patients traveled from as far away as Michigan and Minnesota to UT Southwestern’s Dallas campus to be part of the trial.
Study participants had their T-cells engineered to target a molecule called B-cell maturation antigen, or BCMA, which is only found in plasma cells and myeloma cells. This new T-cell therapy for myeloma patients is called idecabtagene vicleucel, or ide-cel. It is also known as bb2121.
The infusions of the engineered cells started a two-week hospitalization period during which doctors watched for possible side effects such as anemia; neutropenia, a drop in a type of white blood cells; and thrombocytopenia, a drop in blood platelets. Although low blood counts were common, they were manageable, and other severe side effects were uncommon.
“One of the nice things we saw in this study was that the rates of severe CAR T-cell-related toxicities – called neurotoxicity and cytokine release syndrome – were very low in multiple myeloma compared to what we have seen with lymphoma CAR T-cell infusions,” Anderson says. “The majority of people had some side effects, but most were low level and manageable, and I would say this therapy is often much better tolerated than a stem cell transplant, which most of these patients had already gone through.”
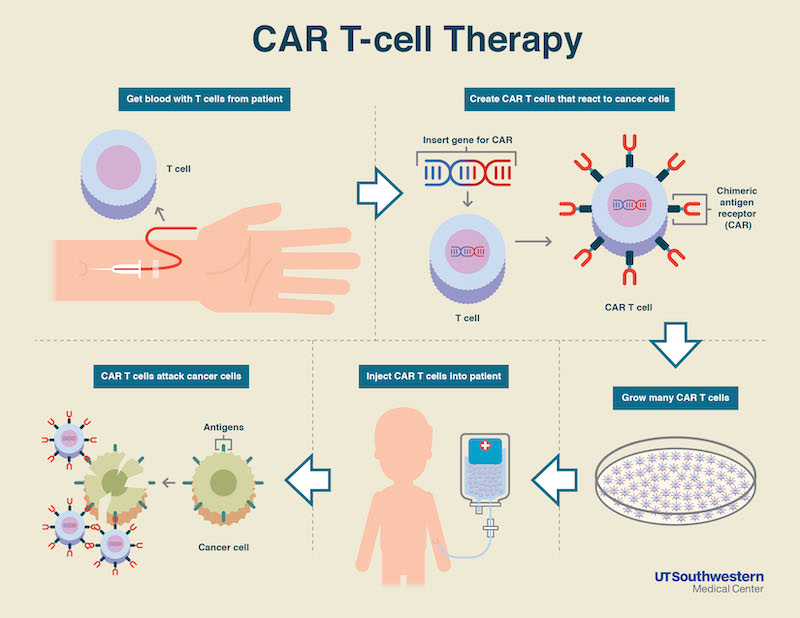
Pioneered in the late 1980s, CAR T-cell therapy is a promising and still emerging treatment for blood cancers. CAR, which stands for chimeric antigen receptor, takes part of its name from the chimera, the mythical animal with the tail of a serpent and head of a lion. In modern medicine’s version of the chimera, the head is an antibody, and the tail is a T-cell receptor. CAR T-cell therapy involves harvesting a patient’s own T-cells by withdrawing blood, reengineering them in a lab to have this cancer-fighting chimera, and then growing hundreds of millions of them to put back into the patient by infusion.
CAR T-cell therapy is currently approved for use only in lymphoma and leukemia. Several different CAR T-cell treatments for myeloma are in clinical trials, but this CAR T-cell treatment is the first to complete and publish data from an FDA registration trial. Based on these results, the pharmaceutical companies Bristol Myers Squibb and bluebird bio are seeking FDA approval of ide-cel as a standard therapy for relapsed myeloma with a decision expected by the end of March.
The trial was funded by bluebird bio and Celgene, a Bristol Myers Squibb company. Anderson is a consultant who serves on an advisory board for Celgene and has other consulting activities disclosed in the manuscript.