Pediatric acute myeloid leukemia or pAML is a childhood blood cancer, one that has proved confounding to clinicians and researchers, with a high relapse rate and relatively few identified genetic mutations (compared to the adult version) that might explain its cause.
In a new study, published in the March 7, 2023 issue of Cell Reports, an international team led by scientists and physicians at University of California San Diego School of Medicine deployed an array of analytical and gene-splicing tools to parse more deeply the mysteries of mutation in pAML.
“Compared to adult AML, pediatric AML is associated with relatively few known mutations, which likely stems from the fact that children have not yet been much exposed to environmental factors that damage DNA,” said senior study author Catriona Jamieson, MD, PhD, professor of medicine, director of the Sanford Stem Cell Institute and a hematologist specializing in blood disorders.
“Our hypothesis was that the drivers were not genomic alterations, but rather occurred within transcriptomic and epitranscriptomic processes.”
The transcriptome describes all of the RNA expressed by genes in an organism, such as a person. RNA is used to convey the genetic (DNA) information needed to make proteins and perform or regulate cellular functions. Transcriptomics is used to learn how genes are turned on and off in different cells and how that may be linked to certain diseases. The epitranscriptome refers to all of the modifications to RNA that occur within a cell.
In their study, Jamieson and colleagues at UC San Diego and in The Netherlands pinpointed a deregulation in splicing — part of the process of decoding gene instructions into proteins — that causes a therapeutic vulnerability to a small molecule splicing inhibitor called Rebecsinib.
In research published last month, Jamieson and colleagues reported that Rebecsinib, an experimental drug, reversed malignant hyper-editing by an inflammation-induced protein known as ADAR1 p150, which promotes immune silencing, metastasis and therapeutic resistance in 20 different cancer types, including leukemia.
“Our findings suggest a new approach to detecting and targeting therapy-resistant leukemia stem cells in pediatric AML and other cancer stem cells that become recalcitrant to treatment as a consequence of this splicing deregulation,” Jamieson said.
About pAML
An estimated 54,000 children and adolescents in the United States are living with or in remission from blood cancers, with leukemia the most common, accounting for more than one-quarter of cases.
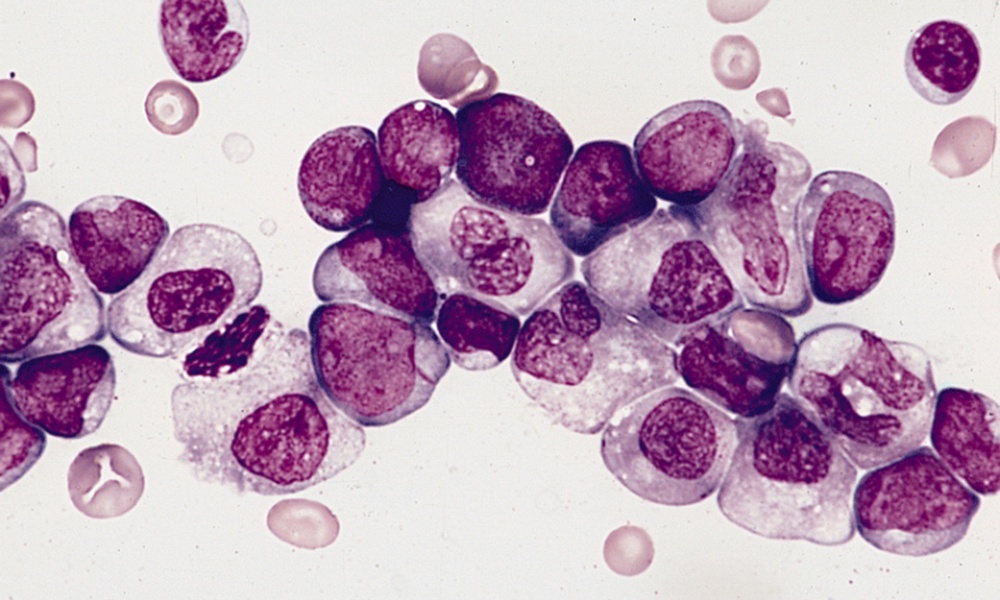
PAML is a type of leukemia in which the bone marrow makes a large number of abnormal blood cells. In healthy children, bone marrow makes blood stem cells that become different types of mature blood cells over time. Myeloid stem cells may become red blood cells that carry oxygen to tissues; granulocytes, which are white blood cells that help fight infections; or platelets that form clots to stop bleeding. Lymphoid stem cells become lymphocytes—white blood cell that are part of the immune system.
The exact cause of pAML is unknown, but children with certain genetic disorders, such as Down syndrome or Fanconi anemia, have been identified as risk factors.
In AML, myeloid stem cells usually become a type of immature white blood cell called a myeloblast. These leukemia cells do not function as healthy white blood cells, but rather accumulate in blood and bone marrow, crowding out healthy cells and leading to infections, anemia or easy bleeding. When AML cells spread outside the blood to other tissues, including the brain, internal organs and skin, they can form solid tumors.
Treatment of pAML has significantly advanced. In the 1980s, almost all children diagnosed with the disease died; today up to 75% survive, but success depends upon comprehensive diagnostics, intensive therapy and effective supportive care. In places where these elements are lacking, survival rates can dip below 50%.
Study co-authors include: Inge van der Werf, Phoebe Mondala, Kathleen Steel, Larisa Balaian, Luisa Ladel, Cayla Mason, Raymond Diep and Jessica Pham, Warren C. Chan, Adam Mark, James J. La Clair, Peggy Wentworth, Kathleen M. Fisch, Leslie Crews, Thomas C. Whisenant, Michael D. Burkart and Mary E. Donohoe, all at UC San Diego; Jacqueline Cloos, Amsterdam University Medical Center; and Gertjan J.L. Kaspers, Princess Máxima Center for Pediatric Oncology and Emma Children’s Hospital, The Netherlands.
Funding and support for this research came, in part, from Padres Pedal the Cause, the National Institutes of Health (grants R01CA205944, R01DK114468-01, 2P30CA023100-28, UL1TR001442), California Institute for Regenerative Medicine (TRAN1-10540), MPN Research Foundation, LLS Blood Cancer Discoveries, NASA (NRA NNJ13ZBG001N), Moores Family Foundation, Koman Family Foundation, Sanford Stem Cell Institute and UC San Diego Moores Cancer Center.
Disclosure: Michael Burkhart is a co-founder of Aspera Biomedicines. Catriona Jamieson is a co-founder of Aspera Biomedicines and Impact Biomedicines, and has received royalties for intellectual property licensed by Forty Seven Inc.
# # #